General Guideline Principles for History Taking and Physical
Examination of Neck Injury for workers compensation patients
The New York State workers compensation board has developed these guidelines to help physicians, podiatrists, and other healthcare professionals provide appropriate treatment for History Taking and Physical Examination of Neck Injury.
These Workers Compensation Board guidelines are intended to assist healthcare professionals in making decisions regarding the appropriate level of care for their patients with ankle and foot disorders.
The guidelines are not a substitute for clinical judgement or professional experience. The ultimate decision regarding care must be made by the patient in consultation with his or her healthcare provider.
History Taking and Physical Examination of Neck Injury
Physical examination and history-taking lay the groundwork for and direct the progression of diagnostic and therapeutic procedures. The objective clinical findings should be given more weight when the results of clinical examinations and those of other diagnostic methods do not agree. The following should be documented in the medical records.
History of Present Injury of Neck Injury
Evaluation and therapy should be based on a thorough history obtained shortly after the accident. The background should contain:
Mechanism of Injury of Neck Injury
- This contains information about how the symptoms started and developed. A thorough account of the occurrence and the body’s position before, during, and after the incident should be included in the mechanism of injury. In the absence of a known incidence, inclusion of work-related body postures, frequency during the workday, and lifting/pushing/pulling needs should be made.
- Location, kind, and aggravating/alleviating elements of your pain (e.g., sleep positions). It’s crucial to determine whether radicular-type symptoms are improved by elevating the arm above the head. Include both the major and secondary complaints in the history (e.g., headaches, primary neck pain, shoulder girdle complaints, and secondary arm pain).
- To ensure that all the symptoms related to the work, including pain, are being treated, it is strongly suggested to utilize an approved pain assessment instrument (e.g., the Visual Analog Scale [VAS]), particularly during the first two weeks after injury.
- Upper and/or lower extremity weakness, numbness, or paresthesia, especially if caused by or made worse by coughing or sneezing.
- Alteration of sexual, genital, or gastrointestinal function.
- Loss or deterioration of fine motor abilities, making it difficult to handle small things
- Past work-related and non-work-related injuries to the same location, including specific prior medical care, a history of specific prior car accidents, persistent or recurrent symptoms, and any functional restrictions. review of any earlier imaging examinations of the spine.
- Previous emotional and/or psychological responses to the accident or sickness at hand.
- Ability to carry out regular tasks and work responsibilities.
History
- Complete surgical and medical history from the past.
- It is important to conduct a system review, which may include signs or symptoms from the following organ systems: integumentary/breast; neurological; psychiatric; hematologic/lymphatic; allergic/immunologic; constitutional symptoms; eyes; ear, nose, and throat; musculoskeletal; genitourinary; gastrointestinal; respiratory; cardiovascular; The scope and focus of the assessment of systems might vary from case to case depending on the underlying ailment being treated and clinical judgment.
- Smoking background.
- Both professional and leisure activities.
- Previous experience with depression, anxiety, or another mental disorder.
- History of cervical injuries, as well as shoulder, arm, forearm, or wrist/hand injuries.
- History of sickness or injury affecting the brachial plexus or upper extremity peripheral nerves
- Walking difficulty and balance issues.
Physical Examination of Neck Injury
Suitable for the subject being assessed, these tests and exam procedures should include:
- visual examination, taking posture into account.
- cervical mobility, flexibility, and the presence of muscular spasms. An examination of a joint’s motion may be necessary. In situations of acute trauma, range of motion should not be assessed until instability and fracture have been ruled out.
- Checking the cervical spine’s atlanto-occipital articulation (upward and downward gaze).
- Identifying myofascial tightness, discomfort, and trigger points by palpating the spinous processes, facets, and muscles.
- Examination of the higher/upper muscle groups’ motor and sensory systems, with an emphasis on their nerve roots, as well as their sensitivity to light touch, pinprick, temperature, position, and vibration A discrepancy of more than 2 cm between the two upper extremities’ circumferences might be a sign of chronic muscle wasting.
- Tendon reflexes deep. Asymmetry could be a sign of disease. The presence of inverted reflexes (such as arm flexion or triceps tapping) may be a sign of spinal cord or nerve root disease at the tested level. The grab reflex, Babinski reaction, lower and/or upper extremity clonus, and Hoffman’s sign are only a few examples of pathologic reflexes.
Relationship to Work of Neck Injury
A declaration about the likelihood that the sickness or injury is work-related is also included in this. If further information is required to assess if the condition is connected to the patient’s job, the doctor should make that known.
Spinal Cord Evaluation of Neck Injury
Additional investigation is necessary when the cause of injury, medical/clinical presentation, or history point to a potentially serious injury. Among the many neurological tests for potential spinal cord damage are:
- Proprioceptive sensory function, temperature, deep pressure, sharp and mild touch.
- Testing for strength.
- Perianal feeling and/or anal sphincter tone.
Abnormal reflexes in the lower and upper extremities of the upper and lower extremities are present.
- Fragmentary Spinal Cord Injury Syndrome Evidence:
- Anterior Cord Syndrome is defined by the retention of touch, vibration, and proprioception together with the loss of motor function, pain perception, and temperature below the level of the lesion. This is frequently observed following a serious compression or flexion injury. To check for a potential reversible compressive lesion needing prompt surgical intervention, an urgent CT or MRI scan is required. The incomplete syndromes have the poorest chances of recovery.
- Ipsilateral motor weakness, proprioceptive disruption, and contralateral changes in pain and temperature perception are the hallmarks of Brown-Sequard syndrome.
- Below the lesion’s level. In situations of lateral mass or penetrating trauma fracture, this is typically observed. Debridement of the open wound may be necessary even when surgery is not particularly required.
- Loss of bowel and bladder function with the maintenance of perianal feeling ng, sensory and motor disruption in all limbs—often the upper than the lower—are characteristics of central cord syndrome. Following hyperextension injuries, this is frequently observed in elderly individuals with spinal stenosis and an inflexible spine. Typically, surgery is not necessary.
- An uncommon disorder called posterior cord syndrome is characterized by intact motor function but the loss of feeling below the level of the damage.
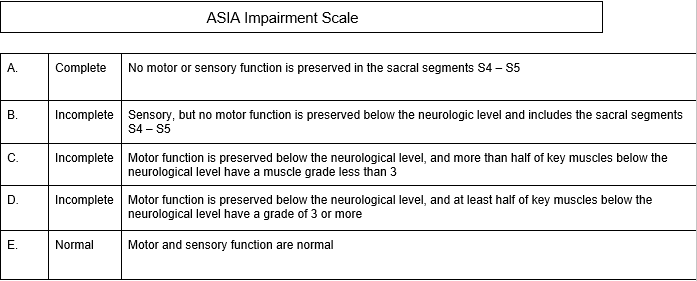
Spinal cord lesions should be classified according to the American Spine Injury Association (ASIA) impairment scale.
Soft Tissue Injury Evaluation of Neck Injury
Traumatic injuries to the muscles, ligaments, tendons, and/or connective tissue are referred to as soft tissue injuries. The most frequent mechanism is abrupt neck hyperextension or hyperflexion.
One of these symptoms may also be caused by lateral acceleration or deceleration. Focused neurological symptoms are not present in a truly isolated cervical strain. Myofascial syndromes, somatic dysfunction, and cervical strain are examples of soft tissue injuries. Soft tissue and more serious cervical injuries can be divided into different categories using the Quebec Classification of Whiplash Associated Disorders:
Grade I
Only neck discomfort, stiffness, or soreness are reported, with no physical symptoms. Muscle spasms are not likely to be caused by the injury. Includes mild cervical sprains, strains, or whiplash.
Grade II
Musculoskeletal symptoms in the neck, such as a restricted range of motion. includes soft tissue injury-related muscle spasms, whiplash, cervical sprain, and cervicalgia, which causes headaches and damaged ligaments and facet joints in the neck.
Grade III
Neurologic symptoms together with neck issues, such as reduced range of motion. includes cervicalgia with headaches, whiplash, cervicobrachialgia, and ruptured disc.
Grade IV
Neck pain accompanied by fracture or dislocation
Red Flags of Neck Injury
Red flags are observations that suggest potentially significant and urgent medical issues. The review of the history and physical examination should involve looking for warning signs. Acute fractures, acute dislocations, infections, tumors, increasing neurological deficits, cauda equina syndrome, and extraspinal illnesses are a few examples of these observations or signs in the cervical spine.
The New York Neck Injury Medical Treatment Guidelines contain modifications in clinical treatment brought on by the existence of “red flags,” and additional evaluation/consultation or urgent/emergency action may be necessary.
What our office can do if you have workers compensation History Taking and Physical Examination of Neck Injury
We have the experience to help you with their workers compensation injuries. We understand what you are going through and will meet your medical needs and follow the guidelines set by the New York State Workers Compensation Board.
We understand the importance of your workers compensation cases. Let us help you navigate through the maze of dealing with the workers compensation insurance company and your employer.
We understand that this is a stressful time for you and your family. If you would like to schedule an appointment, please contact us so we will do everything we can to make it as easy on you as possible.
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.