General Guideline Principles for Hip Osteonecrosis
for workers compensation patients
The New York State workers compensation board has developed these guidelines to help physicians, podiatrists, and other healthcare professionals provide appropriate treatment for Hip Osteonecrosis.
These Workers Compensation Board guidelines are intended to assist healthcare professionals in making decisions regarding the appropriate level of care for their patients with ankle and foot disorders.
The guidelines are not a substitute for clinical judgement or professional experience. The ultimate decision regarding care must be made by the patient in consultation with his or her healthcare provider.
We have extensive experience in treating this condition. You can read more about avascular necrosis and hip avascular necrosis here.
We have answered several questions here about avascular necrosis of the hip and avascular necrosis FAQs.
Hip Osteonecrosis
Related Terms
- Osteonecrosis
- Avascular Necrosis (AVN)
- Aseptic Necrosis
- Ischemic Bone Necrosis
- Ischemic Bone Death
Introduction of Hip Osteonecrosis
Osteonecrosis (aka, avascular necrosis) involves bone death Some cases are regarded as occupational disorders, especially in the context of dysbarism (atmospheric compression/decompression) workers, such as divers and other workers in compressed air environments, who experience a reduced blood supply to the femur as a result of nitrogen gas in the blood during excessively rapid decompression. Another documented cause is severe trauma.
It is believed that significant, discrete trauma poses a risk. Non-traumatic occupational physical aspects, however, are debatable. The focus of treatment is focused on reducing the exposure(s) believed to be at fault.
Sometimes, an osteotomy procedure, vascularized and non vascularized bone grafting, and a surgical “coring” procedure are used. Arthroplasty may be necessary in severe situations.
Diagnostic Studies of Hip Osteonecrosis for workers compensation patients
Initial Assessment
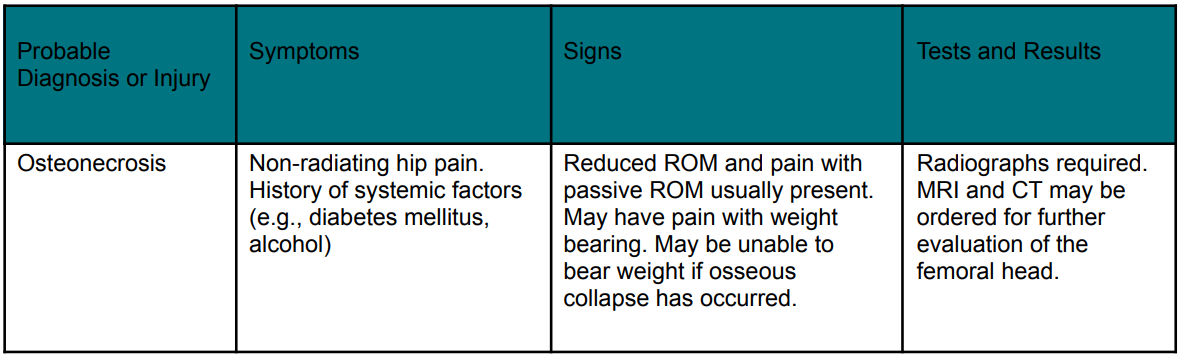
Most hip diseases can be accurately diagnosed using the history, physical exam, and radiographs. The knee, spine, abdomen, and genitourinary tract should all be reviewed during the system reviews and examinations.
Imaging studies are most frequently used to diagnose osteonecrosis. Magnetic resonance imaging (MRI with or without gadolinium, etc.) is typically the imaging of choice if the diagnosis of hip discomfort is still ambiguous following radiographs.
Diagnostic Criteria for Non-Red-Flag Conditions
- Bone Scanning with SPECT is recommended – for select use in patients with acute, subacute, or chronic pain to assist in the diagnosis of osteonecrosis and other conditions with increased polyostotic bone metabolism, particularly when more than one joint needs evaluation.Indications: Bone scanning is mostly used in cases of osteonecrosis since it can be useful in identifying regions of enhanced bone metabolism.Frequency/Dose/Duration: one assessment Bone scan use is Supported by the Data
- CT for Evaluating OsteonecrosisCT for Evaluating Osteonecrosis are recommended for diagnosing patients with osteonecrosis, including those who require advanced imaging but can’t get an MRI or who don’t have access to helical CT.Indications: Thought to be osteonecrosis-related hip discomfort, however MRI is contraindicated.
Frequency/Dose/Duration: Typically, one assessment. If there is a substantial clinical change or to assess progress/resolution, a second assessment may be necessary.
Rationale: When sophisticated imaging of calcified bones is needed for the majority of hip problems, computerised tomography is thought to be preferable to MRI. There is no obvious advantage of CT over MRI for osteonecrosis. However, the use of CT is restricted, even in environments without helical CT, as it is generally believed that helical CT is preferred for the identification of fracturing.
- Helical CT for Evaluating OsteonecrosisHelical CT for Evaluating Osteonecrosis is recommended for assessing patients with osteonecrosis who cannot receive an MRI due to medical reasons.Indications: considered to be caused by osteonecrosis, particularly in light of worries regarding fracture and collapse. Also suggested for people who require an osteonecrosis examination but who cannot undergo an MRI.
Frequency/Dose/Duration: Typically, one assessment. If there is a substantial clinical change or to assess progress/resolution, a second assessment may be necessary.
Rationale: When sophisticated imaging of calcified structures is needed to diagnose most hip problems, helical CT is thought to be better than MRI. There is no obvious advantage of CT over MRI for osteonecrosis. Helical CT is advised for specific applications because it is believed to be more effective than CT at identifying fracture.
- MRI for Diagnosing OsteonecrosisMRI for Diagnosing Osteonecrosis is recommended for subacute or persistent hip pain presumed to be caused by osteonecrosis, especially if the diagnosis is undetermined or if further testing and/or staging are required.Frequency/Dose/Duration: typically one assessment. If there is a substantial clinical change or the need to assess progress or resolution, a second assessment may be necessary.
Rationale: When it comes to detecting bone collapse, helical computed tomography is thought to be superior to MRI. For imaging bone marrow edema, which is inversely linked with prognosis, MRI is thought to be preferable. As a result, each test has benefits.
- X-Rays for Diagnosing OsteonecrosisX-Rays for Diagnosing Osteonecrosis is recommended for all individuals who have osteonecrosis, it is believed.Frequency/Dose/Duration: It is typical to routinely acquire x-rays to monitor the progression of the condition.
Rationale: X-rays are useful for evaluating the majority of individuals with hip pain, both to make a diagnosis and to help narrow down the range of possible diagnoses. X-rays taken at the early stages of osteonecrosis may be normal or somewhat osteopenic. A high degree of suspicion must be maintained.
- Ultrasound for OsteonecrosisUltrasound for Osteonecrosis is not recommended for diagnosing osteonecrosis
Medications of Hip Osteonecrosis
Ibuprofen, naproxen, or other NSAIDs from an earlier generation are suggested as first-line treatments for the majority of patients. For patients who are not candidates for NSAIDs, acetaminophen (or the analogue paracetamol) may be a viable alternative, even if the majority of research indicates it is just marginally less effective than NSAIDs.
There is proof that NSAIDs are less dangerous and just as effective in treating pain as opioids, such as tramadol.
- Non-Steroidal Anti-inflammatory Drugs (NSAIDs) for Treatment of Acute, Subacute, or Chronic OsteonecrosisNon-Steroidal Anti-inflammatory Drugs (NSAIDs) for Treatment of Acute, Subacute, or Chronic Osteonecrosis are recommended for the treatment of severe, mild, or persistent osteonecrosis Warning signs Treatment with NSAIDs is advised for osteonecrosis that is acute, subacute, or chronic. First, try over-the-counter (OTC) medications to see whether they work.Frequency/Dose/Duration: Many patients could find it reasonable to use as needed.
Indications for Discontinuation: Osteonecrosis healing, lack of effectiveness, or the emergence of unfavourable effects that need stopping the treatment.
- NSAIDs for Patients at High Risk of Gastrointestinal BleedingNSAIDs for Patients at High Risk of Gastrointestinal Bleeding is recommended for people at high risk of gastrointestinal bleeding to take misoprostol, sucralfate, histamine Type 2 receptor antagonists, and proton pump inhibitors together.Indications: Cytoprotective drugs should be taken into consideration for patients with a high-risk factor profile who also have indications for NSAIDs, especially if a prolonged course of treatment is planned. Patients who have a history of gastrointestinal bleeding in the past, the elderly, diabetics, and smokers are at risk.
Frequency/Dose/Duration: H2 blockers, misoprostol, sucralfate, and proton pump inhibitors are advised. dosage recommendations from the manufacturer. It is generally accepted that there are no significant differences in effectiveness for preventing gastrointestinal bleeding.
Indications for Discontinuation: Intolerance, the emergence of negative effects, or the stopping of NSAIDs.
- NSAIDs for Patients at Risk for Cardiovascular Adverse EffectsNSAIDs for Patients at Risk for Cardiovascular Adverse Effects is recommended Acetaminophen or aspirin as first-line therapy seem to be the least dangerous in terms of cardiovascular side effects. If necessary, non-selective NSAIDs are recommended to COX-2-specific medications.To reduce the chance that an NSAID will negate the protective effects of low-dose aspirin in individuals receiving it for primary or secondary cardiovascular disease prevention, the NSAID should be taken at least 30 minutes after or 8 hours before the daily aspirin.
- Aetaminophen for Treatment of Osteonecrosis PainAetaminophen for Treatment of Osteonecrosis Pain is recommended for the management of osteonecrosis pain, especially in patients who have NSAID contraindications.Indications: Acute, subacute, chronic, and post-operative osteonecrosis pain in all individuals.
Frequency/Dose/Duration: As per the manufacturer’s recommendations; can be used as required. Over four gm/day, there is evidence of liver toxicity
Indications for Discontinuation: harmful effects of pain relief repercussions or intolerance.
- Opioids of Hip OsteonecrosisOpioids of Hip Osteonecrosis is recommended for brief use (no more than seven days) as an NSAID supplementary treatment.Indications: In order to control pain, a brief prescription of opioids is frequently necessary, especially at night, as an adjuvant to more effective medications (notably NSAIDs, acetaminophen).
Frequency/Dose/Duration: As needed during the day, solely at night thereafter, and finally completely discontinued.
Rationale for Recommendation: When NSAIDs are ineffective in relieving a patient’s pain, opioids should be used sparingly, especially at night. Opioids should only be taken sparingly and briefly, particularly at night to induce sleep.
- BisphosphonatesBisphosphonates are not recommended for treatment of osteonecrosis.
- Anticonvulsant Agents (including Topriamate)Anticonvulsant Agents (including Topriamate) are not recommended for the management of osteonecrosis-related pain.
- Gabapentin and PregabalinGabapentin and Pregabalin is not recommended for osteonecrosis-related discomfort.
- GlucocorticosteroidsGlucocorticosteroids are not recommended in order to treat osteonecrosis.
Treatments of Hip Osteonecrosis
Finding and treating reversible risk factors is the primary focus of early treatment for mild to severe cases of osteonecrosis. It is advised to cut back on or stop doing things that trigger symptoms noticeably, including avoiding dysbaric exposures. Most moderately severe or severe instances are treated surgically right away, especially if a collapse has already taken place.
Initial Care
The initial stage in evaluating osteonecrosis is determining the severity of the condition. Decompression atmosphere removal is a common early intervention. The majority of patients with osteonecrosis-related hip pain may find relief from nonprescription analgesics tolerable. Surgical intervention is necessary if either the illness is getting worse or the condition is advancing.
De/compression is the main activity to be concerned with in cases of acute and subacute osteonecrosis. Decompression treatments shouldn’t often be administered to patients with osteonecrosis until the condition has improved.
In individuals with osteonecrosis (especially those with more severe illness at risk of collapse), high force and/or high impact force (e.g., jumping) should typically be avoided until the condition is either significantly improved or resolved. No matter whether stage of osteonecrosis you have (acute, subacute, or chronic), sticking to the decompression tables is strongly recommended.
Surgery of Hip Osteonecrosis
- Core Decompression SurgeryCore Decompression Surgery is recommended in order to treat osteonecrosis.Indications: individuals with typically moderate to Those with severe osteonecrosis who are either in adjustment of risk factors and/or (ii) perception of risk collapsing and delaying further while addressing danger factors. Treatment with hyperbaric oxygen is seen as being excessively dangerous.
We have significant experience in core decompression and you can read about it here.
We have edicationed others on the subject of avascular necrosis with Dr. Max Gomez.
- Arthroplasty for OsteonecrosisArthroplasty for Osteonecrosis is recommended to treat severe disease that is unresponsive to non-operative treatment or osteonecrosis with collapse.Indications: Patients who have collapsed femoral heads qualify for arthroplasty right away. Those with severe osteonecrosis who are resistant to risk factor adjustment and/or (ii) thought to be at immediate risk of collapse are further prospects.
Rationale: Arthroplasties are frequently used as a treatment once the head of the femur collapses.
Other Treatments of Hip Osteonecrosis
- Dysbaric Exposures or Other Symptom-Providing Activities or Other Risk FactorsDysbaric Exposures or Other Symptom-Providing Activities or Other Risk Factors are recommended reduction or cessation of actions that provide serious osteonecrosis risks, such as avoiding dysbaric exposures.
- Non-Weight Bearing ActivitiesNon-Weight Bearing Activities are not recommended for people who have osteonecrosis.
- Hyperbaric OxygenHyperbaric Oxygen is recommended in order to treat osteonecrosis.Stage 2 of Osteonecrosis Ficat. It might make sense. to try HBO on patients who have osteonecrosis that is more advanced.
Frequency/Dose/Duration: Up to 30 treatments.
Indications for Discontinuation: Course completion, intolerance resolution, clinical resolution, and collapse of osteonecrosis.
What our office can do if you have Hip Osteonecrosis from workers compensation injury
We have the experience to help you with their workers compensation injuries. We understand what you are going through and will meet your medical needs and follow the guidelines set by the New York State Workers Compensation Board.
We understand the importance of your workers compensation cases. Let us help you navigate through the maze of dealing with the workers compensation insurance company and your employer.
We understand that this is a stressful time for you and your family. If you would like to schedule an appointment, please contact us so we will do everything we can to make it as easy on you as possible.
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.