Spinal Fusion vs. Microdiscectomy
If spine pain becomes so severe that it disrupts daily life or is accompanied by swelling, tenderness, or redness, it’s important to seek medical attention.
At Complete Orthopedics, our expert spine specialists are adept at treating spine pain through both surgical and non-surgical means. We examine symptoms, diagnose the condition, and recommend suitable treatments, including surgery if necessary.
Serving New York City and Long Island, we partner with six hospitals to offer cutting-edge spine surgery and comprehensive orthopedic care. You can schedule a consultation with our orthopedic surgeons online or by phone.
Learn about the common causes of spine pain and the treatment options available, including when surgery might be the best choice.
Overview
Spinal fusion and microdiscectomy are surgical procedures used to treat back pain and radiating leg pain due to disease processes in the lower back. The lumbar fusion surgery is done with the goal of naturally joining the two vertebrae together after removal of the intervertebral disc. Microdiscectomy surgery is a minimally invasive surgery used to remove herniated part of the intervertebral disc.
Microdiscectomy is performed mainly for the management of sciatica or lumbar radiculopathy caused by a herniated intervertebral disc. The lumbar fusion surgery may also be performed for lumbar radiculopathy but due to causes such as recurrent disc herniation, multiple disc herniation, instability, spondylolisthesis, lumbar canal stenosis, and in serious diseases such as cancer or infection of the lumbar spine.
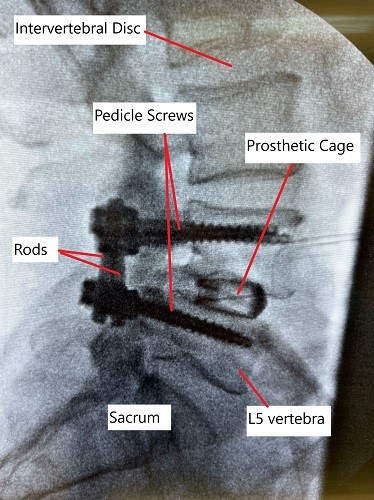
X-ray showing lumbar spine fusion at L4-L5 level.
Lumbar fusion surgery is an extensive surgery as compared to microdiscectomy, though the fusion surgery may also be done with minimally invasive techniques. Lumbar fusion surgery involves an incision either from the front of the abdomen, or the back, or from the sides.
The surgeon proceeds to remove the intervertebral disc and freshen the edges of the adjoining vertebrae. The surgeon also removes any bone spurs and tissues such as longitudinal ligament or ligamentum flavum that may be narrowing the canal. The canal may also be widened with the removal of parts of the lamina and the facet joint.
The surgeon then introduces a prosthetic cage to decompress the segment and maintain the disc space. The cage and the surrounding area of the intervertebral space are filled with bone graft. The bone graft may be harvested from the patient’s pelvic bone or from a bone bank. The surgeon then uses metallic hardware in the form of screws and rods to fasten the fusion construct.
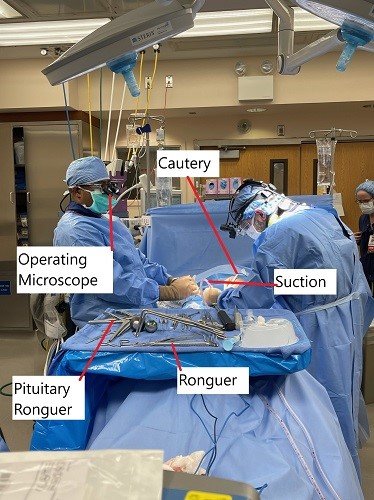
Intraoperative image showing microdiscectomy surgery.
Outcomes
Over the months, the lumbar fusion construct is fused together naturally. The bone construct removes any abnormal movement between the vertebrae.
Microdiscectomy surgery on the other hand involves the removal of just the herniated part of the intervertebral disc. The surgeon uses a small incision in the back and uses an operating microscope to visualize the operating field. The surgeon removes a small part of the lamina to visualize the disc and proceeds to remove the herniated part.
The microdiscectomy is a minimally invasive surgery that may be performed in an outpatient setting under local anesthesia. The lumbar fusion surgery on the other hand is performed under general anesthesia. After microdiscectomy, patients may be able to go home the same day of the surgery but may require an overnight stay at the hospital following lumbar fusion surgery.
Lumbar fusion surgery although can be used for the management of herniated discs, it is only used in cases where disc herniation is associated with instability of the spine. Lumbar fusion is also used in cases where sciatica is caused due to narrowing of the canal known as lumbar canal stenosis. The fusion surgery is also done due to instability of the spine segment after removal of a herniated disc owing to the loss of disc height and diameter.
Patients with spondylolisthesis have an instability of the segment due to slippage of one vertebra over the other. Spondylolisthesis may lead to disc herniation and narrowing of the canal. The instability may be a result of trauma or due to a deformity present since birth. Lumbar fusion surgery helps to stabilize the spine segment.
Microdiscectomy is a highly successful surgery but some patients may have a recurrent disc herniation due to incomplete removal and weakening of the outer ring. Recurrent disc herniation causing sciatica are better addressed by lumbar fusion surgery.
Comparative Outcomes
Recurrent Lumbar Disc Herniation (RLDH) Treatment:
- Re-operative Rates: As noted, RD had higher re-operative rates due to recurrent herniation, while SF’s lower rates were primarily due to complications from adjacent segmental degeneration and implant issues.
- Clinical Improvement: Both procedures showed similar improvements in patient-reported outcomes, with no significant differences in ODI and JOA scores.
- Complications: Complications like dural tears were comparable between the two procedures, highlighting the necessity for surgical precision and postoperative care in both approaches.
Rehabilitation
The rehabilitation following microdiscectomy is short as compared to lumbar fusion. The spine movement of the patient is decreased due to loss of motion about the fused segment. The loss of motion of the involved segment may place extra load over the adjacent segments leading to adjacent segment degeneration.
Further with spinal fusion, in rare cases there may be complications in the form of non fusion, broken hardware or misplaced hardware.
Both microdiscectomy and spinal fusion may be used to address prolapsed intervertebral disc but both have significantly different indications. The decision regarding the type of surgery is based on the patient’s anatomy, disease process and associated conditions. Speak with your spine surgeon to discuss the type of surgery best suited in your case.
Conclusion
In conclusion, the choice between repeat discectomy and spinal fusion for treating recurrent lumbar disc herniation should be tailored to the individual patient’s condition, considering factors like spinal stability, previous surgical outcomes, and overall health. Both procedures have shown to provide significant clinical improvement with comparable complication rates. However, the decision should weigh the benefits of shorter operative time and less invasiveness of RD against the long-term stability provided by SF.
Do you have more questions?
What are the common complications associated with spinal fusion?
Common complications include increased blood loss during surgery, longer operative times, higher overall costs, risk of adjacent segmental degeneration, and potential for implant-related issues.
What are the primary benefits of spinal fusion for recurrent lumbar disc herniation?
The primary benefits of spinal fusion include providing long-term spinal stability, reducing the risk of future herniations at the operated level, and potentially lessening the need for future surgeries.
How do recovery times compare between spinal fusion and microdiscectomy?
Recovery times are generally shorter for microdiscectomy, with patients often resuming normal activities within a few weeks, whereas spinal fusion patients might need several months to fully recover.
Can spinal fusion and microdiscectomy be combined in a single procedure?
Yes, in some cases, a combined approach might be used where microdiscectomy is performed to remove the herniated disc material, followed by spinal fusion to stabilize the segment.
What factors influence the decision between spinal fusion and microdiscectomy?
Factors include the patient’s overall health, severity of spinal instability, previous surgical outcomes, presence of adjacent segmental degeneration, and the specific characteristics of the disc herniation.
What is the likelihood of requiring further surgery after a repeat discectomy?
The meta-analysis indicated a re-operative rate of 9.09% for repeat discectomy, mainly due to recurrent herniation.
What are the long-term outcomes of spinal fusion compared to microdiscectomy?
Long-term outcomes show that both procedures provide similar clinical improvements. However, spinal fusion offers better spinal stability, which might reduce the risk of future herniations at the operated level.
How does blood loss compare between spinal fusion and microdiscectomy?
Blood loss is significantly less in microdiscectomy (around 200-300 ml) compared to spinal fusion (over 500 ml), making microdiscectomy a less invasive option.
Is there a difference in pain relief between spinal fusion and microdiscectomy?
Both procedures provide significant pain relief, though spinal fusion might offer better results for back pain due to its stabilizing effect, while microdiscectomy is more effective for leg pain caused by nerve compression.
What is adjacent segmental degeneration, and why is it a concern with spinal fusion?
Adjacent segmental degeneration refers to the deterioration of spinal segments next to the fused vertebrae, which can occur because the fusion increases stress on these adjacent segments, potentially leading to further issues and surgeries.
What are the typical hospital stays for spinal fusion versus microdiscectomy?
Hospital stays for microdiscectomy average around 3 days, while spinal fusion patients might stay for over 6 days, reflecting the more extensive nature of the fusion surgery.
What are the primary causes for re-operation in spinal fusion?
Re-operations in spinal fusion are mainly due to adjacent segmental degeneration and implant removal issues.
How do operative times compare between the two procedures?
Operative times for microdiscectomy are shorter, averaging around 100 minutes, while spinal fusion procedures often take more than 150 minutes due to the complexity of the surgery.
Can spinal fusion lead to limitations in spinal movement?
Yes, spinal fusion limits movement at the fused segment, which can result in reduced flexibility and potential changes in biomechanics that might affect adjacent segments.
What is the significance of the Oswestry Disability Index (ODI) and Japanese Orthopaedic Association (JOA) scores in these studies?
These scores measure the degree of disability and pain relief. The studies found no significant differences in the improvement of these scores between the two procedures, indicating that both are effective in improving patient outcomes.
What follow-up care is required after spinal fusion or microdiscectomy?
Follow-up care for both procedures includes regular monitoring through physical exams and imaging studies, physical therapy to restore function and strength, and possibly lifestyle modifications to prevent recurrence.
How does patient satisfaction compare between spinal fusion and microdiscectomy?
Patient satisfaction is generally high for both procedures, with no significant differences reported in the studies. Satisfaction often depends on the resolution of symptoms and the absence of complications.
Are there any non-surgical alternatives to treat recurrent lumbar disc herniation?
Non-surgical alternatives include physical therapy, pain management through medications or injections, and lifestyle changes to reduce strain on the spine. However, these might be less effective for severe cases.
What advancements are being made in the surgical treatment of recurrent lumbar disc herniation?
Advancements include minimally invasive surgical techniques, better imaging technologies for precise diagnosis and planning, and the development of improved spinal implants and biologics to enhance fusion and recovery.
How do personal health and lifestyle factors impact the choice between spinal fusion and microdiscectomy?
Factors such as the patient’s age, activity level, overall health, presence of comorbidities, and personal preferences play a significant role in deciding the most appropriate surgical intervention.
What are the costs associated with spinal fusion compared to microdiscectomy?
Spinal fusion generally involves higher costs due to the complexity of the procedure, longer operative times, more extended hospital stays, and the use of implants and other materials. Microdiscectomy is less expensive due to its minimally invasive nature and shorter recovery period.
What is the prognosis for patients undergoing either procedure for recurrent lumbar disc herniation?
The prognosis for patients undergoing either spinal fusion or microdiscectomy is generally good, with most patients experiencing significant relief from symptoms and improved quality of life. The choice of procedure should be tailored to the patient’s specific condition and needs, with close follow-up to monitor for potential complications or recurrence.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

