Microscopic / Endoscopic Discectomy
Radiculopathy due to a lumbar disc herniation is a common problem in the active population. In 90% of the patients, it can be treated conservatively. Surgical management is only required when all conservative management has failed.
Surgical treatment of disc herniation has evolved since 1977 when it was first performed in Europe and 1978 when it was first performed in the US. The surgeries have changed from the use of chemicals like chymopapain to open discectomies followed by microdiscectomy and endoscopic discectomy.
The evolution of surgery has led it to a smaller incision, minimizing morbidity, and maximizing results decreased hospital stay with no significant difference in long-term reoperation rates.
The use of improved instrumentation and better visualization and also the use of an operating microscope has led to the evolution of discectomy to microdiscectomy and endoscopic discectomy.
Microscopic discectomy is a gold standard procedure for lumbar disc herniation. Operating microscope not only helps improve optics but also magnifies and allows it to work with good precision.
The use of loupes and headlight also gives similar results. Because of these advances, microdiscectomy can now be done as an outpatient procedure and same-day surgery.
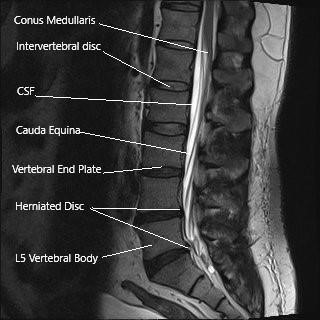
MRI showing sagittal section of the lumbar spine.
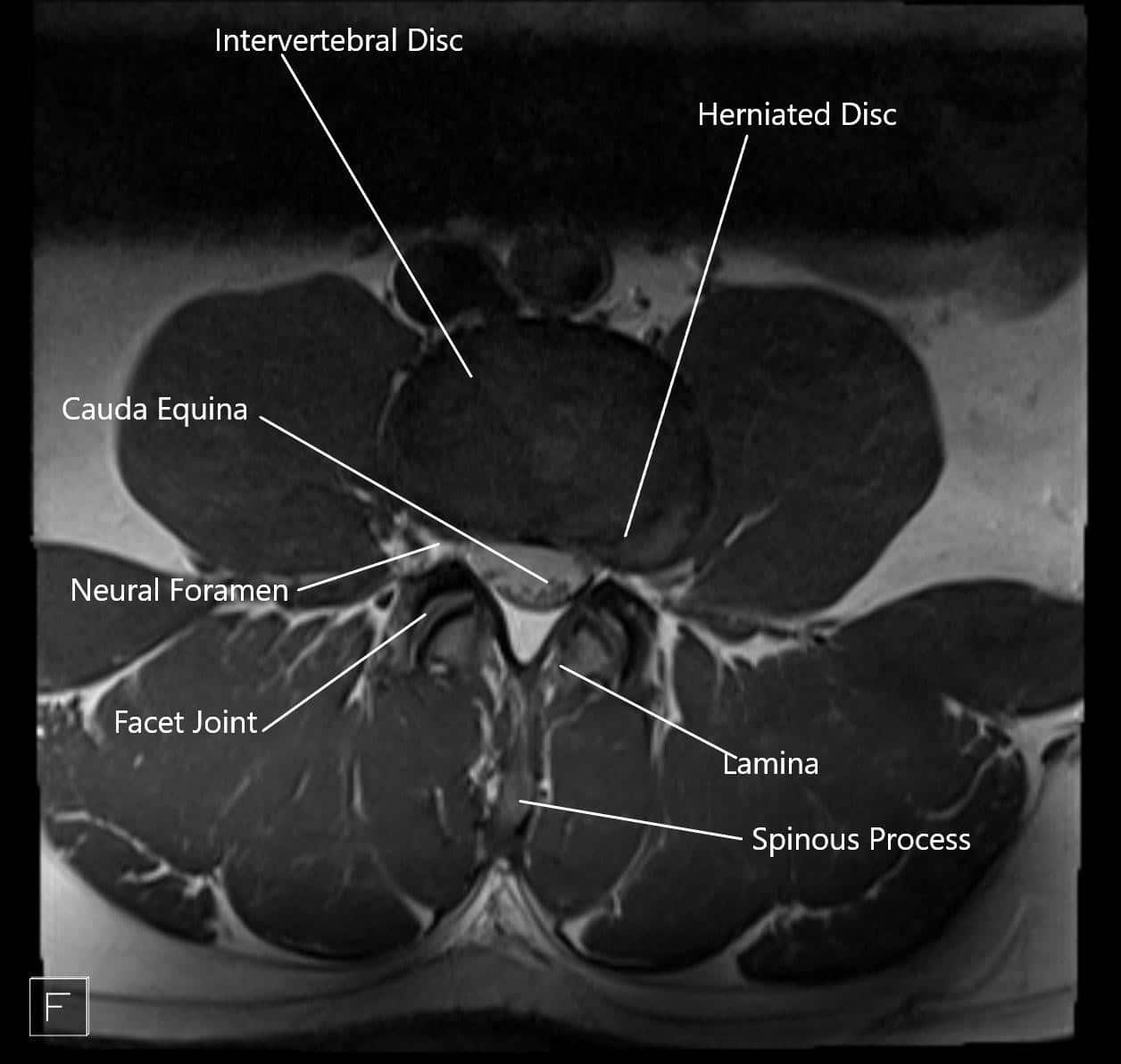
MRI showing herniated disc in axial section.
Indications
Patients with single-level disc herniation with the presentation of radiculopathy with or without tingling or numbness or weakness who have failed conservative means and have documented nerve root compression are ideal patients for microdiscectomy or endoscopic discectomy.
Patients with radicular pain going down their leg, have consistently good results as compared to those who have lower back pain. This pain is caused due to the nerve being pressed by disc herniation.
Patients with cauda equina syndrome or sudden onset worsening neurological deficit are candidates for urgent surgery and may have a guarded prognosis.
Contraindication
Contraindication for microdiscectomy or endoscopic discectomy includes
- Infection
- Tumor
- Gross instability
- Fracture
Technique
After careful selection of the patient for surgery as indicated above, patients are taken to the operating room where they are put under general anesthesia. After anesthesia, the patients are flipped onto their bellies on a special table. All the bony prominences are well padded and the nerves are well padded.
The area of surgery is well-prepped and draped aseptically. X-ray imaging (Fluoroscopy) is used inside the operating room to identify the level before the decision. Once the incision is given, meticulous dissection and hemostasis is achieved and the back of the spine is reached, the level is again checked under x-ray.
For tubular microdiscectomy, a similar approach is performed with the use of sequential dilation and the use of tubes to visualize the area of interest. This requires no muscle stripping and minimal injury to the muscles.
While performing endoscopic discectomy, a camera is used instead of the operating microscope, and the area of surgery is visualized on a monitor. Special instruments are used to the surgery which allows the camera to project as well as perform the surgery.
After confirming the level, some of the bone from the back of the spine is removed to expose the yellow ligament (ligamentum flavum) underneath. The ligament is also excised to expose the nerve roots.
The nerve roots are carefully retracted to the other side to expose the disc herniation. The extruded disc is removed carefully. Once all the loose disc herniation is removed, the nerve roots are checked for any pressure.
After a satisfactory decompression is achieved, hemostasis is achieved and the wound is closed. We also use vancomycin antibiotics in the wound along with hemostatic agents.
The incision for microdiscectomy is usually about 5 cm. Patients usually use a small dressing on their lower back. After the surgery, the patient is flipped onto their back and recovered from anesthesia and moved to the recovery unit.
Once they are awake and up and about, they are discharged to their home. They are sent with pain medications.

Operating room image of the endoscopic/microscopic lumbar discectomy.
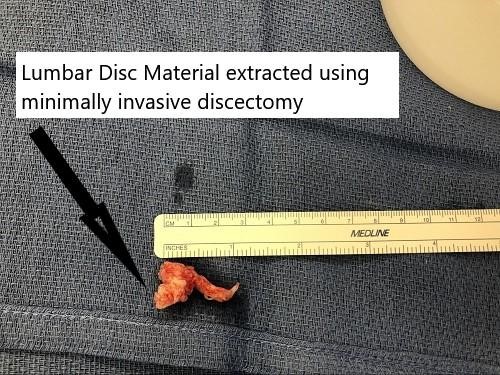
Intraoperative image showing the extracted disc material.

Intraoperative image showing the surgical incision size of minimally invasive lumbar discectomy.
Complications
Though the surgeries are relatively safe surgery, there are still complications that can happen which include injury to the dura, which may need primary repair.
Other complications include injury to the nerve root, hematoma formation, infection, medical complications, a recurrent disc herniation may also occur. Patients who have multiple comorbidities are at higher risk of complications.
Conclusion
Microdiscectomy and endoscopic discectomy are safe and effective procedures, which are needed in about 10% of patients with disc herniation, having failed nonsurgical treatment.
Patients who undergo surgical treatment have better outcomes than patients who underwent non-surgical treatments and are symptomatic in the long-term and allow early return to work.
Do you have more questions?
What is radiculopathy?
Radiculopathy is a condition caused by compression or irritation of a nerve root in the spine, leading to pain, numbness, or weakness radiating along the path of the nerve.
What causes lumbar disc herniation?
Lumbar disc herniation occurs when the inner gel-like core of a spinal disc (nucleus pulposus) protrudes through the outer layer (annulus fibrosus), often due to degeneration, injury, or excessive strain.
How is lumbar radiculopathy diagnosed?
Diagnosis typically involves a physical examination, medical history, and imaging studies such as MRI or CT scans to identify the herniated disc and nerve compression.
What are the symptoms of lumbar radiculopathy?
Symptoms include sharp pain radiating from the lower back down the leg, numbness, tingling, and muscle weakness in the affected areas.
When is surgery considered for lumbar disc herniation?
Surgery is considered when conservative treatments fail to relieve symptoms, or in cases of severe pain, significant neurological deficits, or cauda equina syndrome.
What are the types of surgeries available for lumbar disc herniation?
The main types are microdiscectomy and endoscopic discectomy, which involve removing the herniated disc material to relieve nerve compression.
How does a microdiscectomy differ from an endoscopic discectomy?
Microdiscectomy uses an operating microscope for enhanced visualization and precision, while endoscopic discectomy uses a camera and monitor to perform the surgery with minimal incisions.
What are the benefits of minimally invasive spine surgery?
Benefits include smaller incisions, less muscle damage, reduced pain, shorter hospital stays, and quicker recovery times.
What is the recovery process like after microdiscectomy or endoscopic discectomy?
Recovery involves managing pain, gradually increasing activity levels, physical therapy, and avoiding heavy lifting or twisting movements for a period. Many patients return to normal activities within a few weeks.
What are the risks and complications of lumbar disc surgery?
Potential risks include dural tears, nerve injury, infection, hematoma, recurrent disc herniation, and general surgical risks like anesthesia complications.
What is cauda equina syndrome, and why is it urgent?
Cauda equina syndrome is a severe condition where the bundle of nerves at the end of the spinal cord is compressed, causing severe pain, numbness, weakness, and loss of bladder or bowel control. It requires urgent surgical intervention.
How successful are microdiscectomy and endoscopic discectomy?
Both procedures have high success rates, with many patients experiencing significant pain relief and improved function. Success is often measured by reduced pain and improved quality of life.
Can lumbar disc herniation recur after surgery?
Yes, there is a risk of recurrent disc herniation, though it is relatively low. Maintaining a healthy lifestyle and avoiding excessive strain on the spine can help reduce this risk.
Will I need physical therapy after surgery?
Physical therapy is often recommended to strengthen the muscles, improve flexibility, and support the spine during recovery.
What can I do to prevent lumbar disc herniation?
Preventive measures include regular exercise, maintaining a healthy weight, using proper lifting techniques, avoiding prolonged sitting or standing, and practicing good posture.
How long will I need to stay in the hospital after surgery?
Many microdiscectomy and endoscopic discectomy procedures are performed as outpatient surgeries, allowing patients to go home the same day or after an overnight stay.
Is there a difference in outcomes between surgical and non-surgical treatments?
Surgical treatments generally provide faster and more significant relief of symptoms compared to non-surgical treatments, especially for patients with severe or persistent radiculopathy.
How do you decide which type of surgery is best for me?
The choice of surgery depends on factors such as the location and severity of the herniation, the patient’s overall health, and the presence of any contraindications. Your surgeon will discuss the options and recommend the best approach for your specific condition.
What kind of anesthesia is used during the surgery?
General anesthesia is typically used, ensuring the patient is asleep and pain-free during the procedure.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

