Minimally Invasive Lumbar Fusion
If lumbar spine pain becomes so severe that it disrupts daily life or is accompanied by swelling, tenderness, or redness, it’s important to seek medical attention.
At Complete Orthopedics, our expert lumbar spine specialists are adept at treating lumbar spine pain through both surgical and non-surgical means. We examine symptoms, diagnose the condition, and recommend suitable treatments, including surgery if necessary.
Serving New York City and Long Island, we partner with six hospitals to offer cutting-edge lumbar spine surgery and comprehensive orthopedic care. You can schedule a consultation with our orthopedic surgeons online or by phone.
Learn about the common causes of lumbar spine pain and the treatment options available, including when surgery might be the best choice.
Overview
Lumbar fusion surgery is commonly done to treat a variety of lumbar spine conditions that may be degenerative, traumatic, or tumor-related. With the advancement of minimally invasive surgery (MIS) techniques in other fields of surgery, these techniques are increasingly being used in spine surgeries such as lumbar fusion. Compared to traditional open techniques, the minimally invasive surgery techniques offer faster recovery, less postoperative pain, and fewer complications.

Stand alone interbody spacer used in MIS ALIF.
The Procedure
Lumbar fusion surgery may be performed by either fusion of the vertebrae from the back, front, or sides. Lumbar fusion surgery typically involves the fusion of the adjacent vertebral bodies by removal of the intervertebral disc but may involve only the fusion of the facet joints. The lumbar fusion surgery also involves the removal of any bony or soft tissue structure impinging upon the dural tissue or spinal nerve/roots.
The fusion of the adjacent vertebrae is achieved by placing a bone graft in between the two vertebrae that heals by forming a rigid bone bridge. The height of the vertebrae after removal of the intervertebral disc is maintained by the introduction of a cage along with the bone graft. The cage may be made of metal, plastic polymer, or machined bone graft.
The fusion construct is further stabilized by the addition of screws and rods or plate and screws. The instrumentation of the segment allows the patient the ability to move without compromising the healing bone graft.
The traditional approach to the lumbar fusion construct involves an open approach. The open approach may be done from the front known as an anterior lumbar interbody fusion or from the back known as the posterior lumbar interbody fusion. Both the traditional approaches involve a large incision and cutting of significant tissues to visualize the bony landmarks and removal of compressing tissues.
Although successful, the traditional open approach is being replaced by minimally invasive techniques that achieve the same degree of fusion results. The minimally invasive techniques may be applied to either anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF), or transforaminal interbody fusion (TLIF).
The minimally invasive techniques utilize smaller incisions of about 1-2 inches that may be single or multiple depending upon the procedure. More importantly, rather than the smaller incision, the minimally invasive lumbar fusion involves less cutting of the tissues.
Traditional open surgeries for lumbar fusion involve significant cutting of the paraspinal muscles when performed from the back. The cutting of the paraspinal muscles and their rigorous manipulation during the surgery often results in prolonged back pain and decreased muscle strength after the surgery. The minimally invasive techniques employed in posterior surgeries minimize the trauma to the paraspinal muscles by the use of serial dilators. The serial dilators are introduced and they dilate the space between the paraspinal muscle instead of cutting them.
The open approach from the front is often associated with a greater risk of damage to the major blood vessels and parasympathetic chain of nerves along with the cutting of the tissues to gain exposure. The minimally invasive anterior lumbar interbody fusion minimizes damage to the blood vessels/nerves and involves less cutting of the tissues to achieve fusion.
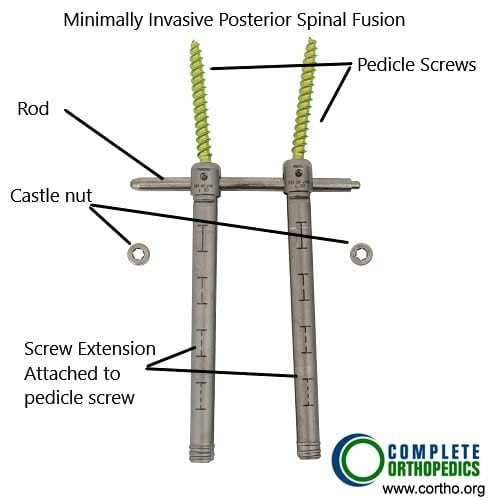
Pedicle screw with cannulated screw extension and castle nut for minimally invasive posterior spine fusion
While performing lumbar interbody fusion from the back using the traditional approach the covering of the nerves known as dural sheath may be damaged. The damaged dural sheath may become scared that may make any future surgery in the area difficult. The minimally invasive surgery circumvents the route for achieving the fusion from the back that has minimum effect on the dural sheath.
Lumbar fusion surgery utilizing a minimally invasive technique involves the use of special instruments and implants. The surgeon uses a microscope/endoscope to illuminate and magnify the narrow field of the surgery. The surgeon uses tubular dilators to retract the soft tissue structures in order to reach the bony landmarks.
Once reaching the bony landmarks, the surgeon then uses the specialized instruments through the tubular dilators to remove parts of the posterior vertebrae and to remove the intervertebral disc. The surgeon then introduces the cage/spacer to maintain disc height along with bone graft material. Similar smaller percutaneous incisions are then used to introduce pedicle screws from the back. The rod on either side is then tightened over the screws to form a solid construct.
After the end of the construct, the operating surgeon withdraws the tubular dilators and the incisions are closed in layers. The procedure may be performed in an outdoor patient setting and the patient may be able to go home the same day of the procedure.
Minimally invasive lumbar fusion may be used to treat a wide range of conditions such as spondylolisthesis, herniated discs, deformity correction, and degenerative lumbar disc disease, etc. The minimally invasive lumbar fusion offers the advantage of less blood loss and lower risk of infection. The less cutting of tissues ensures reduced postoperative pain and less use of analgesics. The patients are able to get back to their day-to-day activities faster than the traditional open lumbar fusion.
Although the minimally invasive lumbar fusion offers various advantages, it is not indicated in every patient, and in some patients, the open approach may be better suited. The orthopedic surgeon attending to the patient will assess the patient’s condition and discuss the type of surgery indicated in his/her case.
Benefits of Minimally Invasive Lumbar Surgery
Reduced Tissue Damage and Postoperative Pain
One of the primary advantages of MIS is the reduced damage to muscles and soft tissues. Smaller incisions and less muscle dissection result in decreased postoperative pain and a quicker return to normal activities. Patients undergoing MIS often experience less postoperative discomfort and require fewer pain medications compared to those undergoing traditional open surgery.
Shorter Hospital Stays and Faster Recovery
MIS techniques are associated with shorter hospital stays and faster recovery times. Many MIS procedures can be performed on an outpatient basis or with a brief hospital stay. The reduced trauma to tissues and lower risk of complications contribute to a quicker recovery, allowing patients to resume their daily activities sooner. The articles reviewed highlight the positive impact of MIS on postoperative recovery, with many patients returning to work and normal life within a few weeks of surgery.
Lower Risk of Complications
The minimally invasive nature of these procedures reduces the risk of complications such as infection, blood loss, and muscle atrophy. The smaller incisions and precise instrumentation used in MIS minimize the exposure of internal tissues to potential contaminants, decreasing the likelihood of postoperative infections. Additionally, the reduced need for blood transfusions and the preservation of muscle function contribute to better overall outcomes for patients.
Improved Cosmetic Outcomes
Smaller incisions and reduced scarring are significant cosmetic benefits of MIS. Patients often appreciate the improved aesthetic outcomes, which can contribute to higher satisfaction with the surgical procedure. The articles underscore the importance of these cosmetic benefits, especially for younger patients and those concerned about the appearance of their surgical scars.
Conclusion
Minimally invasive lumbar surgery represents a transformative approach to the management of lumbar spine conditions. The techniques and technologies associated with MIS offer significant advantages over traditional open surgery, including reduced tissue damage, lower postoperative pain, shorter hospital stays, and improved cosmetic outcomes. However, the adoption of MIS also presents challenges, including a steep learning curve for surgeons, limited indications, and the high costs of advanced equipment.
Do you have more questions?
How do I schedule a consultation with an orthopedic surgeon at Complete Orthopedics?
Consultations can be scheduled online through the Complete Orthopedics website or by calling their office directly.
When can I go back to work after minimal invasive back surgery?
Patients with minimal invasive back surgery have an earlier recovery than patients who undergo open surgeries. These patients can get back to desk-type job within two to three weeks. Patients who are in high demand job may take up to eight to twelve weeks to get back to their normal job, which includes work or sports. Physical therapy and rehabilitation may have a role to play in recovery of these patients.
How soon after the surgery can I start physical therapy?
Patients are not required to start their physical therapy till two weeks after the surgery. After two weeks of surgery, physician reexamination will help in deciding if the patient requires physical therapy or not. Many of the patients do not require physical therapy after the surgery.
Does smoking cause spine problems?
Smoking has proven to cause spine problems, including neck and lower back. At the same time, smoking is detrimental for patients who require spine surgery, especially fusion surgeries. It has been shown that smoking delays spine fusion, as well as lead to higher incidence of nonunion and possible need for revision surgeries.
What if, during my surgery, you encounter a different issue other than expected?
Usually, before the surgery, we discuss with the patient regarding all the possible spine issues that we may expect and how to manage them. If there is an unexpected issue, which has not been discussed earlier, we would go ahead and discuss it with the patient’s relative and treat it accordingly from there. If there is something which can wait, and is not detrimental to the patient, and relatives are not able to make decision on it, we may leave it for a later date to be discussed with the patient after the surgery.
How long is it possible to stay for back surgery?
Most of the patients with back surgery can be discharged within one to four days after the surgery depending on the type of surgery and the type of recovery that they have. Patients who undergo complex spine surgeries may need longer period of hospitalization and recovery.
Which pain medications will I be sent home with? What are the possible side-effects of these prescriptions?
Most of the patients with cervical spine surgery, will be sent with some narcotic pain medication to take care of their pain. These medications do have their multiple side-effects, which may be constipation, nausea, vomiting, impaired judgement, drowsiness, headache. Though patients who are treated with narcotic pain medication for acute pain, mostly do not lead to addiction, but these medications do have addiction potential.
Will you know before the surgery if I need a brace afterwards? If so, will I be fitted for one before the surgery?
Most of the patients with spine surgery do not need a brace. If we expect that the patient will need a brace, we will get the patient pre-fitted with a brace so that it is available immediately after the surgery. Occasionally the need for brace may be decided at the time of surgery. In such cases a brace is arranged in immediate post-operative period.
Will I need any other medical equipment like a walker when I go home? Should I get an adjusted bed or sleep downstairs?
Patient may need other medical equipment like walker or a stick. If that is required, patients are provided with such equipment in the hospital before their discharge and are trained how to use them by the physical therapist and occupational therapist. If the patient needs to use stairs, patients are trained by the physical therapist before they are let go home. If the patient needs an adjustable bed, they are informed about that. That can be done prior to the surgery. It is desirable for patients to stay downstairs for a few weeks if possible.
Who can I call if I have questions after the surgery?
In case patient has routine questions regarding after the surgery or regarding the surgery, they can call the physician’s office and talk to the nurse or secretary or the physician. If they’re not available on the phone, they can leave a voice mail and they will be answered later. In case the patient has a medical emergency, then they should not call the physician office but rather call 911 or get to the hospital ER as soon as possible.
How often will I see you after my surgery?
Patients are usually followed at two weeks, six weeks, three months, six months, and a year after surgery.
What symptoms would warrant a call to your office after the surgery?
If the patient develops problems like chest pain, breathing problems, sudden neurological deterioration, or any other emergency they should call 911, or go to the emergency room directly. Patients who develop worsening pain at the surgery site, discharge from the wound, fever; they should call in the office.
How long should I wait to bathe after the surgery?
Patients are usually asked to avoid bathing, until the incision heals, which may take two to three weeks. Patient can take shower after 72 hours of surgery with an impervious dressing in place. The dressing can be changes if the wound is visibly soaked. Patients are asked not to rub the area of surgery for about two to three weeks. They can gently dab it dry with a towel.
How long will I be out of work?
Patients with low demand work and desk job, can be back to work as soon as three to six weeks after the surgery depending on patient pain control as well as recovery. Patients who are in heavy lifting or control of heavy machinery or handyman job, may take three to four months, or even more to get back to work depending on their recovery from the surgery.
How soon after the surgery can I start physical therapy?
Patients after back surgery are usually started on physical therapy, if they need, depending on physician’s advice, at two to four weeks after the surgery. Many of the patients do not need physical therapy. A decision to go into physical therapy will depend on the surgery as well their recovery.
What if I get an infection?
If the patient has a superficial infection, few days of antibiotics will help heal these infections. Occasionally patient may develop deep infection. In these patients may need IV antibiotics for a longer period. If despite all efforts or in patients with rapid deterioration due to infection, surgery may be needed to help clean off the infection.
How common is surgery?
Most of the patients do not need surgery and can be treated with conservative means. When the patients do not respond to conservative measures, or if they have worsening neurological deficit, or worse pain, they may need surgery.
Will I have irreversible damage if I delay surgery?
Patients who develop neurological deficit in the form of weakness or involvement of bowel or bladder may have irreversible damage if the surgery is delayed enough.
When do I need fusion?
When patient has back pain or has a surgery in which enough bone is removed to destabilize the spine, in these cases patient may need a fusion surgery to stabilize the spine, as well as to alleviate the symptoms.
What are my risks of low back surgery?
General surgical risks of low back surgeries include bleeding, infection, persistence of pain, reversible/irreversible nerve damage leading to tingling, numbness, or weakness down the legs or involvement of bowel or bladder, failure of resolution of symptoms, failure of fusion, failure of implants. Most of the patients can undergo a safe surgery due to the development of vision magnification as well as refined surgical techniques. There are anesthesia risks also associated with this surgery.
When will I be back to my normal activities?
Though these things depend on the type of surgery patient has undergone, patient can usually be progressively back to their normal activities, starting from three to five days from surgery. Patients are encouraged to take care of their activities of daily living, as well as light household activities. Patients can get back to driving once they are free from pain medication and are able to sit for a duration of period for driving, which may take upto 2-3 weeks or more.
What type of surgery is recommended?
The type of surgery depends on the presenting complaint, examination findings, as well as imaging findings in the form of x-ray and MRI. Some patients may need to undergo just discectomy, or laminectomy, while others may need a fusion surgery on their back to relieve their symptoms. To know more about the type of surgery, the patient needs to discuss this with their spine surgeons.
How long will the surgery take?
Spine surgeries like discectomy and laminectomy usually last about one to one and a half hours. Spine fusion surgeries, may take longer periods, up to two and a half to four hours or more. It depends on type of surgery, and as well as the level of spine to be operated upon.
What is degenerative disc disease?
Degeneration means gradual damage of the tissue. Degenerative disc disease represents aging of the disc, either appropriate to the normal age of the patient, or maybe accelerated due to injury or chronic disease, or other factors like smoking, obesity.
What is Lumbar instability?
Lumbar instability means that the spine is not stable and there is excessive abnormal movement between two vertebrae. This is usually diagnosed by imaging in the form of X-rays, CT scan, or MRI of the patients. Instability may lead to compression of nerve roots causing radiculopathy with or without back pain.
What is spinal stenosis?
Spinal Stenosis means narrowing of the spinal canal. It is can be at the cervical or thoracic or lumbar level. Most common spinal stenosis is at lumbar level and it, when narrowed, can compress nerves, causing pain going down the legs, with or without tingling, numbness, weakness, or involvement of bowel or bladder.
What is sciatica?
Sciatica is another name for lumbar radiculopathy, in which patient has pain going down their legs. The pattern of pain depends on the nerve root involved, but the most common is pain going down the outer side of the thigh and leg into the foot.
What is lumbar disc disease? how is this problem diagnosed?
The diagnosis of Lumbar disc disease is made by history and examination of the patient. The confirmation of diagnosis is done by imaging in the form of X-rays and MRI. Occasionally the patient is having contraindication to MRI, patient may need to undergo a CT scan. When a CT scan is done, occasionally the patient may need to get injected with a dye before the CT scan and this is called CT myelography. Occasionally patient may need a CT scan along with MRI also.
When should I consider surgery for the back pain?
Most of the patients get treated with conservative means. In case the patient is not getting relief despite continuous conservative measures, or if there is worsening of pain associated with or without weakness or involvement of bowel or bladder, the patient may need surgical intervention in the form of surgery.
Am I a candidate for minimal-invasive spine surgery?
Some patients are good candidates for minimally-invasive spine surgery and they can get better with that. History, physical examination, as well as special investigations like X-ray and MRI, are needed in order to discuss regarding options of minimal invasive spine surgery. Some patients are not good candidates for minimal invasive spine surgery and doing such a surgery in such patients may lead to non-resolved solution of the symptoms or worsening.
Will I need physical therapy after I get minimally-invasive spine surgery?
Many patients may require physical therapy after spine surgery, including minimally-invasive spine surgery. The decision to go for physical therapy is taken by the spine surgeon and depends on the condition of the patient, as well as the surgery done. Physical therapy may be required for optimal rehabilitation and recovery of strength of the muscles.
What is a minimal invasive TLIF?
TLIF is a usual form of fusion surgery that is done in lower lumbar spine from the back, in which a cage is put between the vertebral bodies, along with screws to enhance the potential body fusion. Minimally-invasive TLIF means to do the surgery through minimally-invasive methods, in which there are multiple small incisions through which the surgery is done. The surgery in such a case has decreased blood loss and early recovery.
Are there any warning symptoms?
Warning symptoms of lumbar disc disease include worsening pain, tingling and numbness, development of weakness, or worsening of weakness, involvement of bowel or bladder in the form of incontinence of urine or stools, presence of fever, unintentional weight loss. In such conditions patients should immediately seek medical attention.
Do you need any tests?
General blood workup is needed in most patients before the surgery. This will include blood counts as well as metabolic profile. Special tests may be needed in some patients if the physician has suspicion of some other disease. Most of the patients will have to undergo X-ray and MRI, or a CT scan before the surgery to confirm their diagnosis.
What are the possible surgical complications from a low back surgery?
Common complications of a low back spine surgery are bleeding, infection, leak of cerebral spinal fluid temporary or permanent neurological deficits, blindness, worsening of pain, failure of fusion, failure of implants. There may be risks due to the anesthesia also.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

