Lumbar Disc Replacement
If lumbar spine pain becomes so severe that it interferes with daily activities or is accompanied by swelling, tenderness, or redness, seeking medical attention is crucial.
At Complete Orthopedics, our expert lumbar spine specialists are skilled in treating lumbar spine pain through both surgical and non-surgical methods. We assess symptoms, diagnose the condition, and recommend appropriate treatments, including surgery if necessary.
Serving New York City and Long Island, we collaborate with six hospitals to provide advanced lumbar spine surgery and comprehensive orthopedic care. You can schedule a consultation with our orthopedic surgeons online or by phone.
Learn about the common causes of lumbar spine pain and the available treatment options, including when surgery might be the best option.
Overview
Lumbar disc replacement surgery is a modern procedure designed to alleviate chronic lower back pain by replacing a damaged intervertebral disc with an artificial one. This surgery offers a potential alternative to the more traditional lumbar spinal fusion surgery, with research ongoing to determine the long-term outcomes of this newer approach.
Understanding the Spine and Intervertebral Discs
The spine, or vertebral column, is a crucial part of the human body. It not only supports our upright posture but also protects the spinal cord, which is a bundle of nerves that transmits signals between the brain and the rest of the body. The vertebral column consists of 33 vertebrae, with intervertebral discs situated between them. These discs act as cushions, absorbing shocks and allowing for flexibility and movement.
An intervertebral disc has two main parts:
- Annulus Fibrosus: The tough, outer layer.
- Nucleus Pulposus: The soft, gel-like center.
With age or injury, these discs can degenerate, leading to conditions such as lumbar degenerative disc disease. As the central nucleus loses water content, the disc height decreases, which can cause the disc to herniate. Herniation occurs when the inner nucleus pushes through the outer layer, potentially compressing nearby nerves and causing pain and other symptoms.
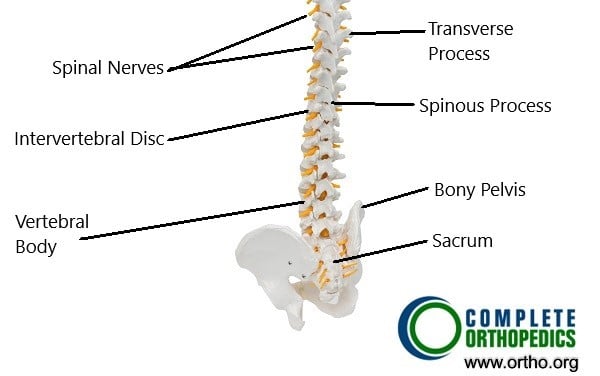 Bone model showing the anatomy of the spine
Bone model showing the anatomy of the spine
With advancing age, the water content of the central nucleus of the disk decreases. As a result of dehydration, the disc height decreases and the intervertebral disk may herniate through the vertebral canal. The herniated disks may compress the dural sac and the transversing or descending spinal nerves. The compression/irritation of the spinal nerves and the dural sac may lead to symptoms of back pain and radiculopathy.
In the majority of patients, these symptoms are relieved in a period of few weeks with conservative management. Conservative management consists of physical therapy, activity modification, pain medications, heat and cold therapy, epidural/nerve block injections, etc.
Conservative Treatment Options
Most people with degenerative disc disease or herniated discs initially undergo conservative treatments, which may include:
- Physical Therapy: Exercises to strengthen the back muscles and improve flexibility.
- Pain Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and sometimes stronger painkillers.
- Activity Modification: Avoiding activities that exacerbate pain.
- Heat and Cold Therapy: Applying heat or ice packs to reduce inflammation and pain.
- Epidural Steroid Injections: Injections to reduce inflammation around the affected nerves.
These treatments are usually effective over several weeks. However, for some patients, these measures may not provide adequate relief.
Surgical Treatment Options
Surgical management is reserved for patients who do not benefit from conservative treatment options for a period of at least 6 months. Spinal fusion is a popular surgical option for such patients. The fusion surgery involved the removal of the herniated disk and insertion of cage with bone graft. The cage and the bone graft help in fusion/welding of the adjoining vertebrae. The surgery often involves supplementation of the fusion with screws and rods to provide stability as the fusion heals.
The fusion surgeries function by elimination the motion between the disease vertebrae and the removal of the disease disk. The procedure is successful in the majority of the patients but some patients may still complain of back pain. The back pain may originate from the loss of the motion of the spine segment. With time, there may be accelerated degeneration of the adjoining spine segments. The adjoining segments degenerate as excess forces act on them due to fusion of a segment.
Lumbar disc replacement was devised to eliminate the shortcomings of the fusion surgery. The artificial disk reproduces the size and the function of the natural disk. The motion of the diseased segment is preserved while the diseased disk is removed.
The artificial disk may be made of surgical grade plastic (polyethylene) or may be made of metal alloys. The artificial disk rests between the surfaces of the adjoining vertebrae that are covered with metal parts.
During the procedure, the surgeon approaches the diseased lumbar vertebrae from the front of the spine. An incision is made in the abdomen and the various organs and blood vessels are gently retracted to reach the lumbar spine. The diseased lumbar intervertebral disk is removed and the ends of the vertebrae are freshened to attach the metal endplates. The artificial disk is introduced and the surgical incision is closed in layers.
The patient may stay at the hospital for 2-3 days and regular activity is permitted after the surgery. Gradually a physical therapy regimen is started to strengthen and improve the flexibility of the back.
Although with it’s advantages over the lumbar fusion surgery, not all patients are candidates for artificial disk replacement. Only patients who are not morbidly obese and with a clear disk pathology are candidates for total disk replacement. Patients with inflammatory bone diseases such as osteoporosis, ankylosing spondylitis, rheumatoid arthritis, etc are poor candidates for disk replacement. Similarly in patients whose back pain is a result of facet joint disease or any infection, tumor, fracture, etc are not candidates for disk replacement.
For patients who do not respond to conservative treatments, surgery may be considered. Traditionally, lumbar spinal fusion has been the go-to surgical option. This involves removing the damaged disc and fusing the adjacent vertebrae together using bone grafts and metal hardware like screws and rods. Fusion aims to eliminate movement between the affected vertebrae, thereby reducing pain. While this procedure is successful for many, it can lead to a loss of flexibility in the spine and may cause accelerated degeneration in adjacent segments.
Lumbar Disc Replacement Surgery
Lumbar disc replacement surgery was developed to address some of the limitations of spinal fusion. Instead of fusing the vertebrae, this procedure involves replacing the damaged disc with an artificial one. The artificial disc is designed to mimic the natural disc’s function, maintaining spinal movement and flexibility.
Materials and Procedure: The artificial disc typically consists of metal and plastic components. During the surgery, the surgeon makes an incision in the patient’s abdomen to access the spine. The damaged disc is removed, and the artificial disc is inserted between the vertebrae. The ends of the vertebrae are prepared to secure the metal plates of the artificial disc.
Recovery: Patients usually stay in the hospital for 2-3 days post-surgery. Physical therapy is gradually introduced to enhance back strength and flexibility. Most patients can return to normal activities within a few weeks.
Candidacy and Potential Complications
Not everyone is a suitable candidate for lumbar disc replacement surgery. Ideal candidates are those with:
- Clear disc pathology
- No significant obesity
- No inflammatory bone diseases like osteoporosis or rheumatoid arthritis
- No facet joint disease, infections, tumors, or fractures causing their back pain
Potential Complications: As with any surgery, there are risks involved, including:
- Excessive bleeding
- Damage to blood vessels or nerves
- Infection
- Implant failure
- Persistent back pain
Conclusion
Lumbar disc replacement surgery represents a significant advancement in the treatment of chronic lower back pain due to degenerative disc disease. By preserving spinal motion and reducing the risk of adjacent segment degeneration, this procedure offers an appealing alternative to spinal fusion. However, careful patient selection is crucial to ensure the best outcomes
Do you have more questions?
Who is a good candidate for lumbar disc replacement surgery?
Good candidates are those with clear disc pathology, not significantly obese, and without inflammatory bone diseases like osteoporosis or rheumatoid arthritis. They should also not have facet joint disease, infections, tumors, or fractures causing their back pain.
How does lumbar disc replacement differ from spinal fusion?
Unlike spinal fusion, which fuses two vertebrae together to eliminate movement, lumbar disc replacement retains the mobility of the spine segment by replacing the damaged disc with an artificial one. This helps maintain natural motion and reduces the risk of degeneration in adjacent segments.
What materials are used in artificial discs?
Artificial discs are typically made from surgical-grade plastic (polyethylene) and metal alloys. The metal parts often cover the surfaces of the adjoining vertebrae, providing stability and durability.
What are the main benefits of lumbar disc replacement surgery?
The main benefits include preserving spinal movement, reducing back pain, and potentially lowering the risk of adjacent segment degeneration compared to spinal fusion.
How long does the surgery take?
The surgery typically takes 2-3 hours, depending on the complexity of the case and the surgeon’s experience.
What are the risks associated with lumbar disc replacement surgery?
Risks include excessive bleeding, damage to blood vessels or nerves, infection, implant failure, and persistent back pain.
What is the recovery time for lumbar disc replacement surgery?
Patients generally stay in the hospital for 2-3 days post-surgery. Full recovery, including a return to normal activities, usually takes several weeks to a few months, with physical therapy playing a crucial role in the rehabilitation process.
How long does the artificial disc last?
Current studies indicate that artificial discs can last 10-15 years or more, but long-term data is still being collected as the procedure is relatively new compared to spinal fusion.
Can a lumbar disc replacement fail?
Yes, like any medical implant, an artificial disc can fail due to factors such as improper placement, wear and tear, or rejection by the body.
What symptoms should prompt me to consider lumbar disc replacement surgery?
Chronic lower back pain not responding to conservative treatments like physical therapy, medications, and injections might prompt consideration for this surgery. Symptoms often include pain radiating down the legs, numbness, and weakness.
How do surgeons determine if a patient is a candidate for this surgery?
Surgeons evaluate medical history, physical examination, imaging studies (like MRI and X-rays), and the response to conservative treatments to determine if a patient is a candidate for lumbar disc replacement.
What is the success rate of lumbar disc replacement surgery?
Success rates are generally high, with many studies showing significant pain relief and improved function. Long-term studies, like the five-year follow-up mentioned, indicate durable benefits with low complication rates.
What should I expect during the recovery period?
Expect a hospital stay of 2-3 days, followed by gradual resumption of activities. Physical therapy will be essential to strengthen your back and improve flexibility. Pain and discomfort are common initially but should decrease over time.
Are there any activities I should avoid post-surgery?
Initially, avoid heavy lifting, bending, and twisting movements. Your surgeon and physical therapist will provide specific guidelines tailored to your recovery progress.
Can I return to work after the surgery?
Many patients return to work within a few weeks, depending on the nature of their job and their recovery progress. Desk jobs may allow an earlier return, while physically demanding jobs may require a longer recovery period.
Will I need physical therapy after the surgery?
Yes, physical therapy is a crucial part of the recovery process, helping to strengthen your back, restore flexibility, and ensure a successful outcome.
Can lumbar disc replacement be performed on more than one disc?
In some cases, multiple discs can be replaced. However, the suitability of multi-level disc replacement depends on individual patient factors and should be discussed with your surgeon.
What are the alternatives to lumbar disc replacement if I am not a candidate?
Alternatives include continued conservative management, spinal fusion surgery, and other less invasive procedures like nerve decompression or spinal injections.
Is lumbar disc replacement covered by insurance?
Coverage varies by insurance provider and policy. It’s essential to check with your insurance company to understand the specifics of your coverage for this procedure.
How do artificial discs compare to natural discs in terms of function?
Artificial discs are designed to mimic the natural disc’s function by allowing motion and providing cushioning between vertebrae. While not identical to natural discs, they offer a similar range of movement and flexibility.
Can I undergo MRI scans after having an artificial disc implanted?
Most modern artificial discs are MRI-compatible. However, it’s essential to inform the radiologist about your implant before undergoing an MRI.
Will I feel the artificial disc in my spine?
Generally, patients do not feel the artificial disc once they have healed. Any initial discomfort typically subsides as the body adjusts to the implant.
What is the long-term outlook for patients with lumbar disc replacement?
The long-term outlook is promising, with many patients experiencing sustained pain relief and improved function. Ongoing research continues to monitor the durability and effectiveness of artificial discs.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

