Juvenile Idiopathic Arthritis
Overview
Juvenile idiopathic arthritis (JIA) is an inflammatory arthritis that affects children aged 16 years or less. The symptoms typically last for 6 weeks or more and a number of joints may be involved including the spine. Juvenile idiopathic arthritis was previously known as juvenile rheumatoid arthritis but it is now known that it is not simply rheumatoid arthritis of the children. The disease encompasses a wide range of symptoms and the cause of JIA is unknown.
Juvenile idiopathic arthritis leads to inflammation of the joints in the body that may cause pain, stiffness, swelling, instability, or loss of function of the joint involved. The facet joints in the spine are synovial joints and the cervical spine is usually affected by juvenile idiopathic arthritis.
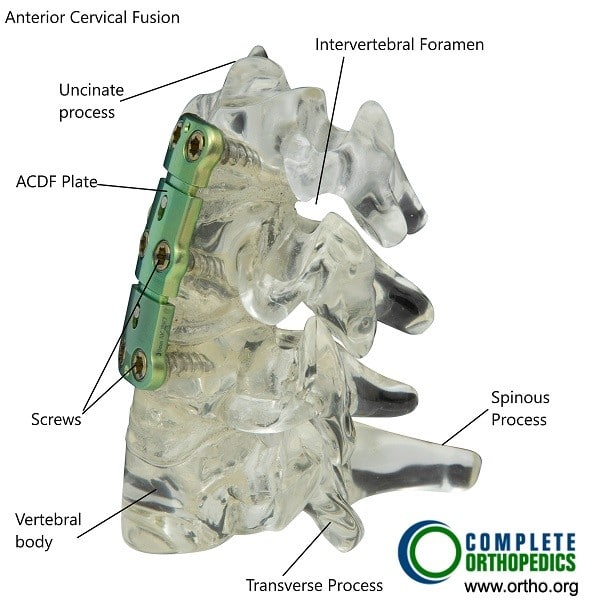
Anterior cervical fusion may be done in severe cases of arthritis and instability of the cervical spine resulting from juvenile idiopathic arthritis.
Symptoms and Impact
JIA leads to inflammation in the joints, causing pain, stiffness, swelling, and sometimes instability or loss of joint function. The condition can affect any joint, including those in the spine, especially the cervical spine (neck area). Symptoms must persist for at least six weeks for a diagnosis of JIA.
Common symptoms include:
- Pain and Stiffness: Particularly noticeable in the morning or after periods of inactivity.
- Swelling and Warmth: Joints may appear swollen and feel warm to the touch.
- Reduced Mobility: Children might struggle with everyday movements, showing signs of limping or avoiding the use of certain limbs.
- Fever and Rash: Some children may experience intermittent fever and rash, particularly in systemic JIA (Still’s disease).
- Eye Inflammation: Conditions like iridocyclitis can lead to blurry vision and, if untreated, vision loss.
Types of Juvenile Idiopathic Arthritis
JIA is categorized based on the number of joints involved and whether other organs are affected:
- Polyarticular JIA: Involves five or more joints, often affecting smaller joints like those in the hands and wrists. It can be severe and resemble adult rheumatoid arthritis.
- Pauciarticular JIA: Involves fewer than five joints, typically larger ones such as the knees and ankles. Eye inflammation is common in this type.
- Systemic JIA (Still’s Disease): Affects multiple joints and other organs like the heart, liver, and spleen. It can present with fever, rash, and swollen lymph nodes.
Diagnostic Process
Diagnosing JIA involves a combination of medical history, physical examinations, and various tests:
- Medical History: Detailed history of symptoms and their progression.
- Physical Examination: Checking joint function and identifying signs of inflammation.
- Blood Tests: To check for markers like rheumatoid factor (RA), antinuclear antibodies (ANA), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). These help rule out infections and confirm inflammation.
- Imaging Tests: X-rays, MRIs, or ultrasounds may be used to assess joint damage.
Treatment Options
Treatment aims to manage symptoms, control inflammation, and prevent joint damage:
- Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): To reduce pain and inflammation.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Such as Methotrexate, Etanercept, Rituximab, and Azathioprine, which slow disease progression.
- Corticosteroids: Used in some cases to control severe inflammation.
- Physical Therapy: Helps maintain joint flexibility and muscle strength.
- Regular Eye Exams: Necessary for early detection and treatment of eye inflammation.
Severe Cases and Surgical Options
In severe cases where joints, particularly in the spine, become highly unstable or damaged, surgical interventions might be required. Anterior cervical fusion is one such surgery performed to stabilize the neck and prevent further damage. Bone-cutting and bone-fusion surgeries might also be considered for children who have reached skeletal maturity and suffer from significant joint damage.
Living with JIA
Managing JIA involves a comprehensive approach, including medication, lifestyle adjustments, and supportive therapies. Key aspects include:
- Regular Exercise: To maintain joint function and overall health.
- Healthy Diet: Ensuring proper nutrition to support growth and immune function.
- Education and Support: For both the child and family to understand the condition and manage it effectively.
Prognosis and Outlook
The outlook for children with JIA varies. With early diagnosis and appropriate treatment, many children lead active, fulfilling lives. Some might experience remission, while others may need long-term treatment and monitoring to manage their symptoms and prevent complications.
Emotional and Psychological Support
Living with a chronic condition like JIA can be challenging for children and their families. Emotional and psychological support is crucial. Support groups, counseling, and educational resources can provide much-needed help and encouragement.
Research and Future Directions
Ongoing research continues to improve our understanding of JIA and develop better treatments. Advances in genetic research and new therapeutic options hold promise for more effective management and potentially a cure in the future.
Conclusion
Juvenile Idiopathic Arthritis is a complex and multifaceted condition that requires careful management and a holistic approach to treatment. By understanding the symptoms, types, diagnostic methods, and treatment options, families can better navigate the challenges of JIA and help their children lead healthy, active lives.
Do you have more questions?
What exactly is Juvenile Idiopathic Arthritis (JIA)?
JIA is a type of arthritis that occurs in children aged 16 or younger. It causes inflammation in the joints, leading to pain, stiffness, and swelling. Unlike adult rheumatoid arthritis, JIA encompasses several types with varying symptoms and severity.
How is JIA different from adult rheumatoid arthritis?
JIA specifically affects children and can have different symptoms and progression patterns compared to adult rheumatoid arthritis. The term “idiopathic” means that the cause is unknown, and JIA includes various subtypes with unique characteristics.
What are the common symptoms of JIA?
Common symptoms include joint pain, swelling, stiffness (especially in the morning), warmth in the joints, intermittent fever, rash, and eye inflammation. These symptoms must persist for at least six weeks for a diagnosis of JIA.
What causes JIA?
The exact cause of JIA is unknown. It is believed to involve a combination of genetic and environmental factors that trigger the immune system to attack the body’s own tissues, leading to inflammation.
How is JIA diagnosed?
Diagnosis involves a detailed medical history, physical examination, and various tests such as blood tests (for markers like RA factor, ANA, ESR, CRP) and imaging tests (X-rays, MRIs) to assess joint damage and rule out other conditions.
What are the types of JIA?
- Polyarticular JIA: Involves five or more joints.
- Pauciarticular JIA: Involves fewer than five joints.
- Systemic JIA (Still’s disease): Affects multiple joints and organs, often presenting with fever and rash.
What are the treatment options for JIA?
Treatment includes medications (NSAIDs, DMARDs like Methotrexate, biologics like Etanercept, corticosteroids), physical therapy, regular eye exams, and in severe cases, surgical interventions.
What medications are commonly used to treat JIA?
- NSAIDs: For pain and inflammation.
- DMARDs: To slow disease progression (e.g., Methotrexate).
- Biologics: Target specific parts of the immune system (e.g., Etanercept).
- Corticosteroids: For severe inflammation.
Can JIA go into remission?
Yes, with early and appropriate treatment, many children can achieve remission, where symptoms significantly reduce or disappear for a period.
How does JIA affect a child’s daily life?
JIA can impact a child’s ability to perform everyday activities due to joint pain and stiffness. It may require adjustments in physical activities and ongoing medical care.
What is the role of physical therapy in managing JIA?
Physical therapy helps maintain joint flexibility, muscle strength, and overall mobility. It is a crucial part of managing JIA.
Are there any lifestyle changes that can help manage JIA?
Regular exercise, a balanced diet, maintaining a healthy weight, and proper rest can help manage symptoms and improve quality of life.
What complications can arise from untreated JIA?
Untreated JIA can lead to joint damage, growth problems, vision loss (due to eye inflammation), and other systemic issues affecting organs like the heart and liver.
What surgical options are available for severe JIA?
In severe cases, surgeries like anterior cervical fusion or joint replacement might be necessary to stabilize or repair damaged joints.
Can JIA cause growth problems in children?
Yes, chronic inflammation and corticosteroid use can affect bone growth and development, potentially leading to growth delays or limb length discrepancies.
How often should a child with JIA see a doctor?
Regular follow-ups are essential. The frequency depends on the severity of the condition but typically involves seeing a pediatric rheumatologist every few months.
Can JIA affect a child’s vision?
Yes, eye inflammation (iridocyclitis) is common, especially in pauciarticular JIA. Regular ophthalmic exams are crucial to prevent vision loss.
Is there a genetic component to JIA?
While the exact cause is unknown, genetics can play a role. Children with a family history of autoimmune diseases may have a higher risk.
Can diet influence JIA symptoms?
A healthy, balanced diet can support overall health, but there is no specific diet proven to cure JIA. Anti-inflammatory foods may help manage symptoms.
What support resources are available for families dealing with JIA?
Support groups, counseling, educational resources, and organizations like the Arthritis Foundation provide valuable information and support.
How can schools accommodate children with JIA?
Schools can make accommodations such as flexible seating, rest breaks, and modified physical activities to support children with JIA.
Are there any new treatments on the horizon for JIA?
Research is ongoing, with new biologics and targeted therapies being developed to improve outcomes and reduce side effects.
What should parents do if they suspect their child has JIA?
Seek medical advice from a pediatrician or pediatric rheumatologist as early diagnosis and treatment are crucial for managing the condition effectively.
What is the long-term outlook for a child with JIA?
With appropriate treatment and management, many children with JIA can lead active, fulfilling lives. Early intervention and adherence to treatment plans are key to improving long-term outcomes.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

