Cervical Corpectomy Surgery
If neck discomfort becomes severe enough to disrupt daily activities or is accompanied by swelling, tenderness, or redness, it is essential to seek medical attention.
At Complete Orthopedics, our skilled spine doctors specialize in treating cervical spine and neck pain using both surgical and non-surgical methods. We evaluate symptoms, identify the cause, and suggest the most suitable treatments, including surgery if necessary.
We serve the New York City and Long Island areas, partnering with six hospitals to offer cutting-edge cervical spine surgery and comprehensive orthopedic care. You can arrange a consultation with our orthopedic surgeons either online or by phone.
Learn about common causes of neck pain and the treatment options available, including when surgery is the best course of action.
Overview
Cervical corpectomy is a surgery that involves the removal of the vertebral body and the intervertebral disc to relieve pressure off the spinal cord and/or the spinal nerves. Corpectomy surgery is a more extensive surgery as compared to the traditionally performed anterior cervical discectomy and fusion.
The spinal cord runs from the base of the brain inside a canal formed by the consecutive vertebrae. At each level, spinal nerves branch from the spinal cord to supply various regions of the body. The intervertebral discs are soft tissues present between two adjoining vertebrae. The intervertebral discs function to cushion the various movements about the spine.
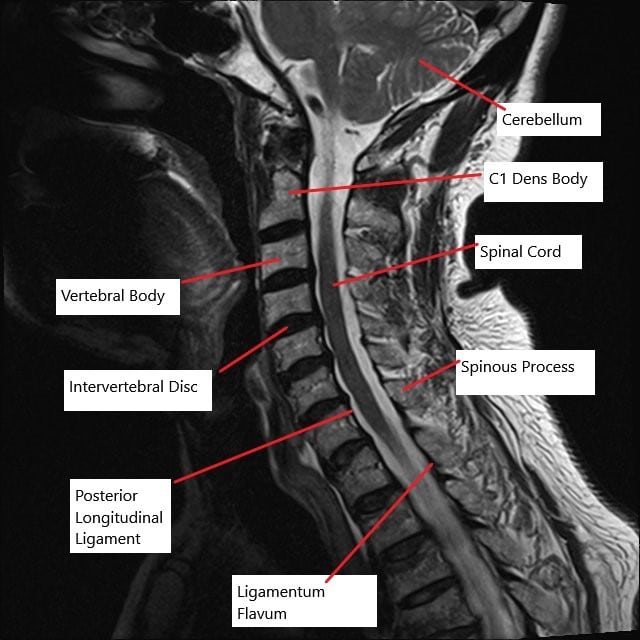
MRI of the cervical spine in the sagittal section showing multiple bulging intervertebral discs.
Indications
The corpectomy surgery is usually indicated secondary to severe compression of the spinal cord or/and spinal nerves. Degenerative disc disease involves the age-related wear and tear of the cervical spine.
The bone spurs may form secondary to the degenerative changes that may cause the compression of the neural structures. There may be stenosis or narrowing of the space available for the spinal nerves or the spinal cord, a condition known as cervical spinal stenosis.
The narrowing and compression of the spinal cord and/or nerves may lead to neck pain associated with numbness and tingling that may travel down to the shoulders, arm, and hands. In severe compression of the spinal cord, there may be a weakness of the upper extremities, including weakness of the hands. In some cases, there may be an associated weakness of the lower extremities and loss of bowel/bladder control.
Besides, the degenerative conditions and cervical spine stenosis, there may be compression of the spinal cord and/or nerves secondary to cervical vertebral fracture or tumor of the vertebral body. The corpectomy surgery is only indicated when all other methods of conservative treatment have been tried and failed. In cases where the pain is severe, or there is a neurological deficit in the form of weakness of the hands or bowel/bladder incontinence, surgery is indicated.
Types of Corpectomy
Anterior Cervical Corpectomy and Fusion (ACCF):
-
- Anterior Approach: The surgeon accesses the spine from the front of the neck.
- Fusion: Bone grafts and plates are used to stabilize the spine after the vertebra is removed.
- Advantages: Less post-operative pain and quicker recovery times.
- Considerations: Suitable for multi-level decompressions but involves delicate dissection around vital structures like the esophagus and carotid arteries.
Posterior Total Laminectomy:
-
- Posterior Approach: The spine is accessed from the back.
- Laminectomy: Removal of the lamina (the back part of the vertebra) to relieve pressure.
- Advantages: Provides a broad decompression area.
- Considerations: Larger incisions and more post-operative discomfort compared to anterior approaches.
Procedure
After appropriate examination, the anesthesiologist numbs the patient in the form of general anesthesia. During general anesthesia, the patient sleeps while the surgery is performed.
The spine surgeon gives an incision in front of the neck, either on the right or the left of the midline. The surgeon carefully retracts the muscles, and the various nerves and blood vessels to reach the front of the involved cervical segment.
Intraoperative fluoroscopy is used to determine the correct level and somatosensory evoked potentials are used to monitor the nerves. The surgeon then removes the intervertebral discs above and below the level of the involved vertebra. A cutting tool is used to remove the attachments from the back of the vertebra.
The vertebral body is removed along with any other tissue which may be impinging upon the spinal cord/spinal nerves. The decompression is followed by the introduction of a bone graft. A solid strut bone graft is usually used which may be harvested from the patient’s own body during the same surgery.
The autologous strut bone graft is usually harvested from the front of the pelvic bone. In addition to the bone graft, a metallic or ceramic bone cage may be introduced to maintain the space occupied by the removed vertebra. A bone graft may also be taken from a bone bank or a man-made bone graft substitute may be used.
The spine surgeon may then introduce a metallic plate in front of the cervical spine to provide stability. The metallic plate is fastened to the adjoining vertebrae with the help of screws. Additional metallic hardware may be introduced from the back to provide more stability to the construct. The stability is checked again with the help of intraoperative fluoroscopy and the incision is closed in layers.
Complications
As with any major surgery, there may be potential complications such as bleeding, infection or blood clots. Additionally, there may be subsidence of the bone graft or the cage. There may be incomplete fusion or no fusion at the corpectomy level. The hardware may break and there may be damage to the nearby blood vessels or nerves.
Recovery Process
Recovery from a corpectomy can vary based on individual factors, including the patient’s overall health, the extent of the surgery, and adherence to post-operative care instructions. Here is a general outline of the recovery process:
Hospital Stay: Patients typically stay in the hospital for a few days post-surgery to monitor for complications and manage pain.
Pain Management: Pain is managed through medications, and patients may have a drain in place to remove excess fluids.
Physical Therapy: A critical component of recovery involves physical therapy to restore mobility and strengthen neck and back muscles.
Activity Restrictions: Patients are advised to avoid heavy lifting, twisting, and bending for several weeks to months. Driving is usually restricted until the patient has regained adequate neck mobility and is off pain medications.
Follow-Up: Regular follow-up appointments are necessary to monitor the fusion process and ensure proper healing.
Long-Term Outcomes
Studies have shown that patients undergoing corpectomy generally experience significant relief from pain and neurological symptoms. Improvement in motor and sensory function, as well as quality of life, is common. Regular monitoring and adherence to post-operative care are crucial for the best outcomes.
Conclusion
Corpectomy is a critical surgical procedure for patients with severe spinal cord compression due to various conditions. It offers significant relief from symptoms and improves the quality of life when other treatments fail. Understanding the procedure, recovery process, risks, and benefits helps patients make informed decisions about their spinal health. Regular follow-up and adherence to recovery protocols are essential for achieving the best possible outcomes.
Do you have more questions?
What are the primary conditions that necessitate a corpectomy?
Corpectomy is primarily indicated for conditions such as cervical spondylotic myelopathy, spinal cord compression due to trauma, severe degenerative disc disease, and tumors affecting the vertebral bodies.
How is the decision made between an anterior and a posterior approach for corpectomy?
The decision depends on the location and extent of the spinal cord compression, the patient’s anatomy, and the presence of previous surgeries or scar tissue. Anterior approaches are preferred for single or multilevel decompressions at the front of the spine, while posterior approaches are used for more extensive decompressions.
What preoperative tests are required before undergoing corpectomy?
Preoperative tests typically include MRI and CT scans to assess the spine’s condition, blood tests to evaluate general health, and sometimes electrodiagnostic studies to assess nerve function.
How long does the corpectomy surgery take?
The duration of the surgery can vary but typically ranges from 3 to 5 hours, depending on the complexity and number of levels involved.
Are there non-surgical alternatives to corpectomy?
Non-surgical treatments include physical therapy, pain management, and lifestyle modifications. However, these are usually insufficient for severe cases requiring corpectomy.
What types of anesthesia are used during corpectomy?
General anesthesia is used, ensuring the patient is unconscious and pain-free throughout the procedure.
How is the removed vertebral body replaced during the surgery?
The removed vertebral body is typically replaced with a bone graft or a synthetic cage filled with bone graft material, which is then secured with metal plates and screws.
What are the main risks associated with corpectomy?
Risks include infection, bleeding, nerve damage, non-fusion of the bone graft, and complications related to the hardware used for stabilization.
How do surgeons avoid damaging the spinal cord during corpectomy?
Surgeons use advanced imaging techniques, careful surgical planning, and precise microsurgical tools to minimize the risk of spinal cord damage.
What measures are taken to prevent infection during surgery?
Surgeons follow strict sterilization protocols, administer prophylactic antibiotics, and use sterile techniques to reduce the risk of infection.
What can patients expect immediately after surgery?
Patients can expect to stay in the hospital for a few days for monitoring, pain management, and initial physical therapy.
How is post-operative pain managed?
Pain is managed through medications such as opioids, NSAIDs, and muscle relaxants, alongside other methods like ice therapy and gradual mobilization.
When can patients resume normal activities after corpectomy?
Patients can typically resume light activities within a few weeks, but heavy lifting and strenuous activities should be avoided for several months. The exact timeline depends on individual recovery.
What are the signs of complications that patients should watch for?
Signs of complications include increased pain, redness or swelling at the incision site, fever, numbness, or weakness. Patients should contact their surgeon immediately if they experience any of these symptoms.
Will patients need physical therapy after corpectomy?
Yes, physical therapy is an essential part of recovery to restore strength, flexibility, and function in the neck and back muscles.
Are there any long-term lifestyle changes required after corpectomy?
Patients may need to adopt ergonomic practices, avoid high-impact activities, and maintain a healthy weight to prevent further spinal issues.
How effective is corpectomy in relieving symptoms and improving quality of life?
Studies have shown that corpectomy is highly effective in relieving pain and neurological symptoms, with most patients experiencing significant improvements in quality of life.
What follow-up care is required after corpectomy?
Follow-up care includes regular visits to the surgeon, imaging studies to monitor fusion, and adherence to physical therapy and activity restrictions.
Can corpectomy be performed minimally invasively?
While traditional corpectomy is an open procedure, minimally invasive techniques are being developed but are not yet widely adopted due to their complexity.
How do surgeons handle multiple level compressions during corpectomy?
Surgeons may perform multilevel corpectomies or combine corpectomy with other procedures like discectomy to address multiple compressions.
What role does patient age play in corpectomy outcomes?
Age can affect recovery, with younger patients generally healing faster. However, older patients can still achieve good outcomes with proper post-operative care.
Are there any dietary recommendations post-surgery?
A balanced diet rich in protein, calcium, and vitamin D can support bone healing. Patients should also stay hydrated and avoid smoking, as it impairs bone healing.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

