Cervical Spondylotic Myelopathy
If cervical spine discomfort becomes intense enough to interfere with daily routines or is joined by swelling, sensitivity, or redness, it’s crucial to obtain medical help.
At Complete Orthopedics, our proficient cervical spine physicians are experts in managing cervical spine discomfort through surgical and non-surgical approaches. We assess symptoms, pinpoint the issue, and recommend appropriate treatments, including surgery if needed.
We serve New York City and Long Island and collaborate with six hospitals, providing leading-edge cervical spine surgery and extensive orthopedic services. You can schedule a consultation with our orthopedic surgeons online or via phone.
Explore common reasons for cervical spine pain and the available treatment options, including when opting for surgery is most recommended.
Overview
Cervical Spondylotic Myelopathy or CSM is a condition in which the spinal cord is compressed or pinched in the neck or the cervical spine due to the aging process. The cervical spondylotic myelopathy happens due to the degeneration or wear and tear of the cervical spine due to their aging process. This can happen at one or multiple levels.
Patients with congenital stenosis of their cervical spine may be predisposed to this condition. These patients have a smaller diameter of the spinal canal since birth. The immediate effects of CSM may be precipitated by a subtle trauma overlying cervical stenosis and the aging process.
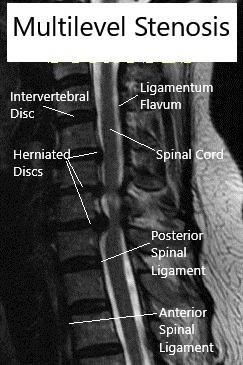
MRI (Sagittal) Cervical spine with multilevel stenosis
As opposed to cervical radiculopathy in which the patient has tingling, numbness or weakness of a specific nerve root presenting in the upper extremity, CSM can present with involvement of either one or to all four extremities.
The involvement can be in the form of sensory deficit and weakness with or without the involvement of gait, bowel or bladder with tingling and numbness all over the body or presenting with electric shock-like sensations going down the body. These patients may even present with inability to ambulate without aid or support. Subtle findings may be an imbalance or subclinical retention of urine.
Causes of Cervical Spondylotic Myelopathy:
CSM is essentially caused due to the aging process leading to wear and tear of the cervical spine. The presentation may be more profound or early in patients with congenital cervical stenosis. The wear and tear lead to degeneration of the disc space with protrusion of the disc towards the spinal cord.
At the same time, the degeneration will lead to thickening of the ligament of the back of the spinal cord called the ligamentum flavum which also contributes to the compression or squeezing of the spinal cord in the neck. This compression of the cord can cause a direct effect over the spinal cord as well as have an indirect effect by decreasing the blood supply to the nerves.
Presentation Signs And Symptoms of Cervical Spondylotic Myelopathy
The patients with Cervical Spondylotic Myelopathy patients may or may not have neck pain. They may present with varied signs and symptoms involving either extremities, bowel or bladder function, or gait abnormalities. These patients may also have a loss of dexterity of their hands or an imbalance of their posture.
On examination by a physician, these patients may elicit inability to walk in a straight line, numbness in specific dermatomes, increased tone of the muscles either upper or lower extremities or spasticity, weakness of specific muscle groups specially hand grip and presentation of electric shock-like sensation or deep flexion of the neck which is also known as the Lhermitte sign.
These patients can present with specific presentations like Central cord syndrome, Brown Sequard Syndrome, Anterior Cord Syndrome, partial or complete spinal cord injury, etc.
Diagnosis of Cervical Spondylotic Myelopathy
After a thorough history and physical examination, an initial X rays may help us know about the degenerative changes in the cervical spine as well as look for evidence of fracture, subluxation, or dislocations.
Patients will usually require advanced imaging to confirm the diagnosis as well as to know the pathology and exact level or levels involved. Magnetic Resonance Imaging (MRI) helps to look at the soft tissue, disc, ligaments, etc. and is the investigation of choice in these patients.
Computed Tomography (CT Scan) is helpful in understanding the bony anatomy of the spine and may also be needed. In patients who are not able to undergo MRI (presence of a pacemaker, aneurysmal clips, etc.) may need to undergo myelography.
Electromyography and urinary bladder studies may be helpful in milder or subtle patients to understand the severity of disease and to help decide the best course of treatment for the patient.
Treatment Options of Cervical Spondylotic Myelopathy:
The patients with mild and early presentations can be treated conservatively and followed closely for the development of any worsening of the symptoms. These patients can be followed by a spine surgeon or a neurologist. Some medications can be helpful in the symptoms. At the same time, physical therapy can also help in strengthening muscles, balance as well as keeping the neck movement at an optimum level.
The course of CSM is that of gradual worsening in most patients but there are patients who can stay stable for a long time. These patients may have sudden rapid worsening in the presence of subtle trauma or even without that.
The patients with severe CSM present with weakness, the involvement of hand dexterity, the involvement of gait, bowel, bladder, spasticity or increased tone of muscles, and usually need surgical treatment in the form of decompression of the cervical spine.
The treatment includes removing off the pressure causing compression and pinching of the spinal cord. The surgery can be performed from the front or the back of the neck. A decision to perform it from the front or back is dependent on multiple factors. Also, the surgery can be fusion or non-fusion surgery.
If the patient has good neck alignment, minimal or no neck pain, minimal or no instability then these patients can be a good candidate for non-fusion surgery like laminoplasty or Total disc replacement.
On the contrary, if the patient has more neck pain, poor neck alignment then an anterior fusion surgery or posterior fusion surgery may be needed. This fusion surgery can be done from the front or the back. If multiple levels are involved then the back surgery may be better especially in patients with proper alignment.
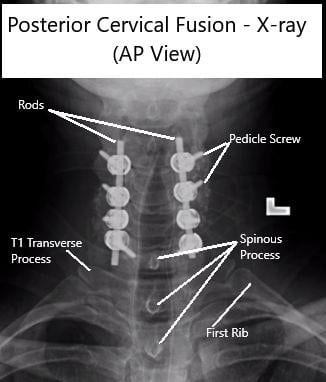
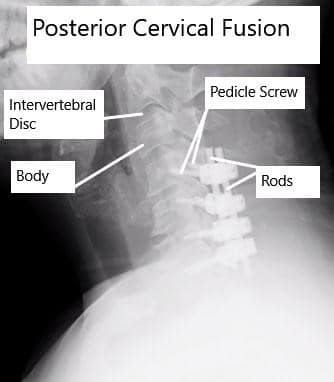
AP and Lateral View X-rays of Posterior Cervical Laminectomy and Fusion
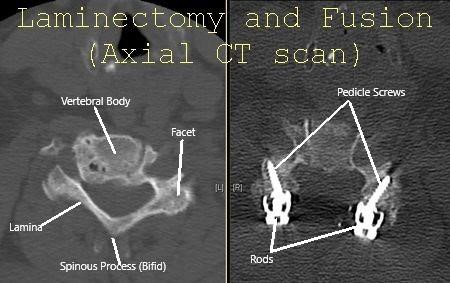
Cervical Spine Axial CT scan showing Laminectomy and fusion.
Patients who need fusion surgery, need to be stabilized by the use of plates, screws, and rods. Once the compression is removed, the worsening of symptoms can be alleviated with an expectancy of recovery over a period of time. Patients usually have to go rehab especially if they are considered weak and are not able to perform the activity of daily living by themselves. These spine surgeries may be associated with complications.
Prognosis of Cervical Spondylotic Myelopathy
The patients with mild involvement can be treated conservatively (without surgery) but need regular follow up and constant supervision under the care of a spine surgeon. These patients may have a stable period with slow and gradual worsening. Occasionally patients may do very well with conservative treatment.
Patients who do not show progressions and are treated early in the process have a fair to a good prognosis. They usually recover near to the complete functions as well as become symptom-free.
The patients who present with severe symptoms or rapid worsening have a poorer prognosis and may not be able to recover full functions and may have residual weakness, spasticity, the involvement of gait, bowel or bladder, and hand dexterity. It may take months and years to recover and rehabilitate for CSM.
Risks of Cervical Spondylotic Myelopathy Surgery:
The patients who undergo surgery for CSM have usual risks of orthopedic surgery which include infection, bleeding, failure of implants, need for repeat surgery. There is a risk of breakdown of adjacent segments with a need for extension of the fusion by another surgery.
The patients also have risks for injury to the nerves or spinal cord leading to a temporary or permanent worsening of functions, inability to recover completely, and regain full functions.
Surgery of the cervical spine also carries a risk of worsening of neurological status which may also lead to the involvement of respiratory functions needing treatment in the form of intubation and ICU support and even death.
As with any spine surgery, the patients are also at risk of blindness, stroke, cardiac events, paralysis, or death. The patient can also have secondary complications to their impaired neurological status like bedsores, lung problems like atelectasis and pneumonia, blood clots or deep vein thrombosis, pulmonary embolism, urosepsis, and even death.
Recovery and Rehabilitation
Postoperative recovery from CSM surgery can vary based on the type of surgery performed and the individual patient’s condition. General guidelines for recovery include:
- Hospital Stay: Most patients stay in the hospital for a few days after surgery. During this time, they are monitored for any complications.
- Pain Management: Pain is managed with medications, and a gradual return to normal activities is encouraged.
- Physical Therapy: Rehabilitation exercises help restore neck mobility, strengthen muscles, and improve overall function. The therapist may also provide guidance on posture and ergonomic adjustments to prevent future problems.
- Follow-Up Appointments: Regular follow-ups with the surgeon are crucial to monitor healing and ensure that the spine is stable.
Long-Term Outlook
The long-term outlook for patients with CSM varies. Many patients experience significant improvement in symptoms following surgery, especially if the condition is treated early. However, some patients may continue to have residual symptoms, such as mild weakness or numbness, particularly if the spinal cord has been severely compressed for a long period before treatment.
It is important for patients to maintain a healthy lifestyle, engage in regular exercise, and avoid activities that could exacerbate neck problems. Regular medical check-ups are also recommended to monitor the health of the cervical spine.
Conclusion
Cervical spondylotic myelopathy is a progressive and potentially debilitating condition that results from age-related changes in the cervical spine. Early recognition and treatment are essential to prevent significant neurological impairment. While non-surgical treatments may be effective for mild cases, surgical intervention is often necessary for moderate to severe CSM to relieve spinal cord compression and improve patient outcomes. If you experience symptoms such as persistent neck pain, numbness, or weakness in your limbs, it is important to seek medical advice to explore potential causes and appropriate treatments. Regular follow-up and adherence to a rehabilitation program can significantly enhance the quality of life for individuals affected by CSM.
Do you have more questions?
What are the early signs of cervical spondylotic myelopathy?
Early signs of cervical spondylotic myelopathy (CSM) often include neck pain, stiffness, and subtle changes such as tingling or numbness in the arms and hands. Patients may also experience slight balance issues or difficulty with fine motor tasks, such as buttoning a shirt or writing.
How quickly does cervical spondylotic myelopathy progress?
The progression of CSM varies widely among individuals. Some may experience a rapid decline in function, while others may have a slow, insidious onset of symptoms over many years. Regular monitoring and early intervention are key to managing the disease effectively.
Can lifestyle changes help manage cervical spondylotic myelopathy?
Yes, lifestyle changes can play a significant role in managing CSM. Maintaining good posture, using ergonomic tools, avoiding heavy lifting, and engaging in regular low-impact exercises can help alleviate symptoms and potentially slow the progression of the condition.
Are there any non-invasive treatments for cervical spondylotic myelopathy?
Non-invasive treatments for CSM include physical therapy to strengthen neck muscles and improve flexibility, pain management with medications such as NSAIDs or muscle relaxants, and lifestyle modifications like improving posture and using cervical collars to support the neck.
When is surgery necessary for cervical spondylotic myelopathy?
Surgery is typically considered necessary for CSM when symptoms are moderate to severe, when there is significant spinal cord compression visible on imaging studies, or when non-surgical treatments fail to provide adequate relief. Surgery aims to decompress the spinal cord and stabilize the spine.
What are the risks associated with surgery for cervical spondylotic myelopathy?
As with any surgical procedure, there are risks associated with surgery for CSM. These can include infection, bleeding, nerve damage, spinal cord injury, complications from anesthesia, and the potential need for further surgeries. However, for many patients, the benefits of surgery outweigh these risks.
How successful is surgery for cervical spondylotic myelopathy?
Surgery for CSM is generally successful, with many patients experiencing significant relief from symptoms. The extent of recovery can vary depending on the severity and duration of spinal cord compression prior to surgery, as well as the patient’s overall health.
Can cervical spondylotic myelopathy recur after surgery?
While surgery aims to decompress the spinal cord and stabilize the spine, there is always a possibility of recurrence. Factors such as ongoing degenerative changes in the spine or inadequate initial decompression can contribute to the recurrence of symptoms.
What kind of rehabilitation is required after surgery?
Rehabilitation after surgery for CSM typically involves physical therapy to improve neck mobility, strengthen muscles, and enhance overall function. This may include guided exercises, posture correction, and possibly occupational therapy to help with daily activities.
How long does recovery take after surgery for cervical spondylotic myelopathy?
Recovery time after surgery for CSM varies but generally ranges from several weeks to months. Most patients can return to normal activities within 3-6 months, depending on the type and extentof the surgery, the patient’s health, and adherence to rehabilitation protocols. Individual recovery can differ, and some patients might experience a quicker return to normal activities, while others might take longer to fully recover.
What are the potential complications if cervical spondylotic myelopathy is left untreated?
If left untreated, CSM can lead to severe and permanent spinal cord damage, resulting in significant neurological deficits such as chronic pain, pronounced muscle weakness, loss of sensation, and severe difficulty in walking or performing daily activities. In extreme cases, it can lead to paralysis or severe disability.
Are there alternative therapies for managing cervical spondylotic myelopathy?
Yes, alternative therapies such as acupuncture, chiropractic care, and yoga might provide some symptom relief for certain patients. However, these should complement, not replace, conventional medical treatments. It is crucial to discuss any alternative therapies with a healthcare provider to ensure they are safe and appropriate for the condition.
Can cervical spondylotic myelopathy affect other parts of the spine?
While CSM specifically affects the cervical spine, the degenerative processes causing it can also impact other parts of the spine, such as the thoracic or lumbar regions. This can lead to similar conditions, like lumbar spondylosis, which can cause lower back pain and nerve compression.
Is cervical spondylotic myelopathy hereditary?
There can be a genetic predisposition to developing spinal degenerative diseases, including CSM. However, environmental factors, lifestyle choices, and occupational hazards also significantly contribute to the condition’s development.
Can cervical spondylotic myelopathy be prevented?
While aging and genetic factors cannot be controlled, certain measures can help reduce the risk of developing CSM. These include maintaining a healthy weight, avoiding smoking, practicing good posture, using ergonomic furniture and tools, and engaging in regular exercise to strengthen the neck and back muscles.
How does cervical spondylotic myelopathy affect daily life?
CSM can significantly impact daily life by causing pain, stiffness, and neurological deficits. These symptoms can make it difficult to perform routine activities, affect work productivity, and reduce overall quality of life. In severe cases, it can lead to loss of independence and the need for assistance with daily tasks.
What is the difference between cervical spondylosis and cervical spondylotic myelopathy?
Cervical spondylosis refers to the general degenerative changes in the cervical spine, such as disc degeneration, bone spur formation, and ligament thickening. Cervical spondylotic myelopathy occurs when these changes compress the spinal cord, leading to neurological symptoms.
Can physical activity worsen cervical spondylotic myelopathy?
High-impact or strenuous physical activities that strain the neck can worsen CSM symptoms. It is essential to engage in low-impact exercises, such as swimming or walking, and follow medical advice on safe physical activities to avoid exacerbating the condition.
How is cervical spondylotic myelopathy different from a herniated disc?
A herniated disc occurs when the soft inner material of a disc bulges out through a tear in the outer layer, potentially compressing nearby nerves or the spinal cord. CSM involves broader degenerative changes that result in spinal cord compression from multiple sources, such as disc herniation, bone spurs, and ligament thickening.
Can cervical spondylotic myelopathy cause cognitive issues?
While CSM primarily affects motor and sensory functions, severe cases can indirectly impact cognitive function due to chronic pain, discomfort, and decreased quality of life, leading to issues like difficulty concentrating, memory problems, and emotional stress.
What role does age play in the development of cervical spondylotic myelopathy?
Age is a significant factor in developing CSM, as degenerative changes in the spine naturally occur with aging. Individuals over 50 are more likely to experience these changes, leading to an increased risk of spinal cord compression and CSM.
Can cervical spondylotic myelopathy be detected through routine check-ups?
CSM might not be detected during routine check-ups unless specific symptoms are reported. Detailed neurological examinations and imaging studies, such as MRI or CT scans, are necessary to diagnose CSM accurately.
What advancements are being made in the treatment of cervical spondylotic myelopathy?
Advances in CSM treatment include minimally invasive surgical techniques, improved imaging technology for early detection, and research into regenerative therapies aimed at repairing spinal cord damage and halting the progression of degenerative changes.
How does cervical spondylotic myelopathy impact mental health?
Chronic pain and disability from CSM can significantly affect mental health, leading to anxiety, depression, and decreased quality of life. Psychological support, counseling, and sometimes medications are necessary to help manage these mental health issues.
Is it safe to drive with cervical spondylotic myelopathy?
Driving can be challenging for individuals with severe CSM symptoms affecting coordination, strength, and reaction times. It is essential to consult with a healthcare provider to assess driving safety and, if necessary, make adjustments or consider alternatives to ensure safety.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.