Anatomy of the Cervical Spine:
Upper Limb Tension Test
Overview
The clinical test known as the Upper Limb Tension Test (ULTT) is presently utilized to distinguish between pain arising from neuromeningeal tissue and pain arising from other structures in the upper limb.
Elvey (1980) initially described the test as a blend of passive shoulder girdle depression, glenohumeral abduction beyond the coronal plane, forearm supination, and wrist extension.
The fundamental test position can be enhanced by incorporating cervical side flexion. If the patient’s symptoms are replicated upon assuming the ULTT position, it suggests involvement of the neuromeningeal tissue.
A positive ULTT result can be confirmed if the symptoms decrease with ipsilateral wrist flexion or worsen with contralateral cervical side-flexion.
The relationship between the biomechanics of the ULTT and the replication of the patient’s symptoms remains ambiguous. Determining the exact source of the patient’s symptoms, such as the cervical spinal nerve, dura, or cords of the brachial plexus, based on the ULTT alone is challenging.
According to literature, the test generates a growing tension in the peripheral nerves that is conveyed to the sheaths of the cervical nerve roots. The C5 and C6 roots of the brachial plexus are the most susceptible to experiencing tensile stresses.
In some cases, When performed with a contralateral limb flexion (CLF), the ULTT induces greater strain in the lateral cord and certain segments of the subclavian artery compared to an ipsilateral limb flexion (ILF).
Types of ULTTs
Median Nerve ULTT: This test targets the median nerve, which runs down the arm and into the hand. It’s often used to diagnose conditions like carpal tunnel syndrome.
Ulnar Nerve ULTT: This test focuses on the ulnar nerve, running along the inner arm and into the fingers, often tested in cases of cubital tunnel syndrome.
Radial Nerve ULTT: This test assesses the radial nerve, which runs along the back of the arm and controls the triceps and wrist extensors.
How ULTTs Are Conducted
During a ULTT, a clinician will carefully move your arm into various positions:
Shoulder Abduction: Lifting the arm sideways.
Elbow Extension: Straightening the elbow.
Wrist and Finger Extension: Pulling the wrist and fingers back.
Neck Movements: Bending or rotating the neck to increase nerve tension.
These positions put stress on specific nerves. If a nerve is compressed or irritated, these movements will likely reproduce the symptoms, such as tingling, numbness, or pain.
Practical Implications
Diagnosis: ULTTs provide a non-invasive, cost-effective method to diagnose nerve issues in the upper limbs. They help pinpoint the affected nerve and guide treatment plans.
Treatment Planning: Understanding which nerve is affected can help healthcare providers design targeted treatment strategies, such as physical therapy or ergonomic adjustments.
Preventive Care: Regular use of ULTTs in clinical settings can help identify early signs of nerve compression, allowing for preventive measures to avoid more severe issues.
How to Prepare for a ULTT
If you’re scheduled for a ULTT, here are some tips to prepare:
- Wear Loose Clothing: This allows easy access to your arms and neck.
- Stay Relaxed: Tension can affect the accuracy of the test.
- Communicate: Inform the clinician about any discomfort or pain during the test.
Anatomy
The interpretation of the impact of forces generated by the ULTT on the cervical spine and brachial plexus based on anatomical studies of cervical nerves may differ between literature, but most of it agrees that the anterior and posterior roots of a nerve emerge from the dura mater independently, each enclosed within its own dural sleeve.
The dura mater is dorsally covered by delicate epidural tissue that spreads laterally to form part of the coverings of the spinal nerves. The fascia of the posterior longitudinal ligament (PLL) spreads outward to connect with the dural root sleeves laterally. This fascia then contributes to the development of the spinal nerve covering.
There has been some uncertainty regarding the level of attachment of the cervical nerves to the adjacent zygapophyseal joints and intervertebral foramina. While literature suggests that nerves are connected to the walls of the foramina through connective tissue, others have argued that such attachments are nearly absent.
However, one researcher found that there may be some exchange of fibers between the nerve sheath and the capsule of the adjacent intervertebral joint, particularly in the anterior region (likely referring to the uncovertebral joint). It has been described that there is a strong connection between the cervical nerves and their adjacent zygapophyseal joints.
The transverse processes’ gutters provide an anchor for the cervical nerves. The connections between the transverse processes and the fifth, sixth, and seventh cervical nerves are referred to as “fibrous slips,” “fibrous attachments,” or specialized “semiconic ligaments.”
The primary anatomical structure that prevents the avulsion of cervical nerve roots is the specialized attachment between the cervical nerves and the transverse process. The dural root pouch is attached to a fascial extension of the posterior longitudinal ligament, which then extends through the intervertebral foramina (IVF) to contribute to the formation of the periradicular covering.
The superficial layer of the posterior longitudinal ligament is the only part that extends laterally as a connective tissue membrane to enclose the nerves, and then it transitions into the connective tissue membrane that surrounds the spinal nerves as they exit the intervertebral foramina.
Gross Anatomy
Essentially, the path and connections of the CS, C6, and C7 within the IVF and the transverse processes of the cervical spine are the same. Dense white fibrous tissue connects much of the circumference of CS, C6, and C7 to the bony margins of their respective IVFs, including the posterior zygapophyseal joint capsule, as these three nerves emerged from the IVF.
The lower surfaces of the nerves do not have this dense attachment of connective tissue. The nerves are only loosely connected to the pedicle below and, for CS and C6, to the transverse process’s gutter floor.
The anterior aspects of the nerves are blended into the epineurium by a thick fascia that extends laterally through the IVF from the posterior longitudinal ligament (PLL). The nerves flattened anteroposteriorly and pass behind the vertebral artery as they exit the IVF. Dense irregular connective tissue fibers can be observed between the nerves and the vertebral artery.
The nerves have a relationship with the vertebral artery in which on its inner side, the vertebral artery is attached by narrow pieces of dense and irregular connective tissue from its outer layer not only to the C5, C6, and C7 cervical vertebrae but also to the intervertebral discs located between C5 and C6, and C6 and C7.
The adventitial coat of the vertebral artery on its lateral side is connected to the anterior surface of the nerves C5, C6, and C7 by connective tissue fibers. The lateral movement of the vertebral artery can be induced by pulling the nerves in a lateral direction.
The displacement of the artery laterally seems to be restricted by the attachments of the artery’s medial side to the periosteum of the vertebral bodies of C5 and C6, and the intervertebral disc of C5 and C6.
As the nerves C5 and C6 travel towards the periphery within the gutter, they are attached to the anterior and posterior edges of the gutter of the transverse processes by bundles of connective tissue. These bands are distinct clusters of tightly-packed connective tissue.
The connective tissue bundles are primarily found on the posterior gutter wall, and their thickness is greatest at the medial end of the gutter. There exist only a limited number of fragile connective tissue strands linking the nerves and the floors of the bony gutters.
Histology
The histological findings reveal the connections of the lower cervical nerves as they exit the spinal cord and move towards the outer regions. Each nerve has its own dural sleeve that contains both its ventral and dorsal root, and the dura is penetrated separately by each of them.
The surrounding structures are connected to the dural sleeves. Anteriorly, there is a thick and dense connective tissue that stretches from the posterior longitudinal ligament (PLL) to the anterior aspect of the dura, particularly in the area where the roots emerge from their dural sleeves.
The layer of membranous tissue extending laterally from the ligament attaches to the posterior aspects of the vertebral bodies and intervertebral discs. The PLL’s lateral extensions pass underneath the ventral root and connect the nerve root to the intervertebral foramen’s floor.
The posterior aspect of the dura is blended with connective tissue fibers extending from the inferior pedicle. The dorsal root ganglion is situated posterior to the vertebral artery in a lateral direction. It is firmly attached to the artery by dense, irregularly arranged connective tissue.
The lower cervical nerves have multiple connections to innervated structures as they travel from the spinal cord to the outside of the spinal cord region:
The anterior surface of the dorsal root ganglion medial to the vertebral artery is attached to connective tissue fibers that extend from the PLL.
At the medial end of the foramina, the nerves attach to the periosteum of the inferior pedicles and the capsules of the zygapophyseal joints by dense connective tissue, posteriorly. The PLL extends laterally to attach the nerves to the vertebral bodies and intervertebral discs anteriorly.
The extensive attachment of the lower cervical nerves to their surrounding structures implies that pain caused by an ULTT is unlikely to be solely derived from neuromeningeal tissue. The lower cervical nerves are attached to many innervated structures.
The sinuvertebral nerve is a composite nerve, consisting of a somatic root from a ventral ramus and an autonomic root from a gray ramus communicantes. The intervertebral discs, PLL, and the periosteum of the ventrolateral spinal canal are all innervated by the sinuvertebral nerve. The cervical dorsal ramus splits into a medial branch which supplies the zygapophyseal joints.
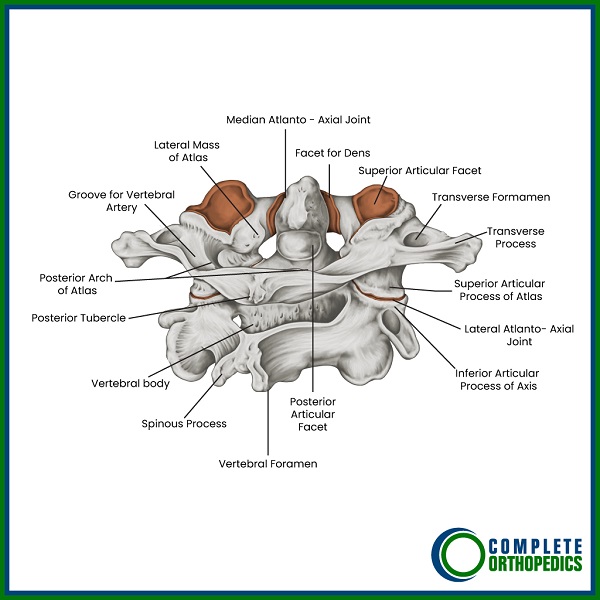
The Atlas (Top Bone in the Cervical Spine) Illustrated
Conclusion
Upper Limb Tension Tests are valuable tools in diagnosing nerve issues related to the cervical spine and upper limbs. They offer a quick and efficient way to identify problems, guiding effective treatment plans. The studies highlight the importance of validating these tests to ensure they provide accurate and reliable results. Understanding the anatomy and biomechanics of the cervical spine and upper limbs is crucial for healthcare providers to utilize ULTTs effectively.
Do you have more questions?
How does the cervical spine contribute to overall spinal health?
The cervical spine supports the head, enables a wide range of movements, and protects the upper part of the spinal cord, playing a crucial role in maintaining posture and facilitating neurological functions.
Can cervical spine issues cause headaches?
Yes, problems in the cervical spine, such as tension or irritation of the nerves, can lead to headaches, often referred to as cervicogenic headaches.
How can poor posture affect the cervical spine?
Poor posture, especially forward head posture, can strain the cervical spine, leading to muscle imbalances, pain, and long-term degenerative changes.
What are cervical spine ligaments, and what do they do?
Cervical spine ligaments, such as the anterior and posterior longitudinal ligaments, support the vertebrae, maintain stability, and limit excessive movement.
How does aging affect the cervical spine?
Aging can lead to degenerative changes such as disc wear (degenerative disc disease), formation of bone spurs (cervical spondylosis), and reduced flexibility and strength in the cervical spine.
What is cervical radiculopathy?
Cervical radiculopathy occurs when a nerve root in the cervical spine is compressed or irritated, leading to pain, numbness, or weakness radiating from the neck into the shoulder, arm, or hand.
What imaging techniques are used to diagnose cervical spine problems?
Common imaging techniques include X-rays to assess bone structures, MRI to visualize soft tissues like discs and nerves, and CT scans for detailed bone imaging.
How can lifestyle changes help prevent cervical spine problems?
Maintaining good posture, regular exercise, ergonomic adjustments, a balanced diet, and avoiding smoking can help prevent cervical spine problems by keeping the spine healthy and strong.
What is the function of the atlas and axis in the cervical spine?
The atlas (C1) supports the skull and allows nodding motion, while the axis (C2) has a peg-like structure called the dens, enabling the head to rotate.
What are the symptoms of cervical myelopathy?
Symptoms of cervical myelopathy, a condition where the spinal cord is compressed, include neck pain, numbness or tingling in the arms and hands, difficulty with coordination, and sometimes bowel or bladder dysfunction.
How does cervical spine surgery help?
Cervical spine surgery can relieve pressure on the spinal cord or nerves, stabilize the spine, and correct deformities, leading to pain relief and improved function.
What are the risks of cervical spine surgery?
Risks include infection, bleeding, nerve damage, non-union of the bones, and complications from anesthesia, though these are relatively rare with modern surgical techniques.
Can cervical spine problems affect balance?
Yes, severe cervical spine issues can affect balance and coordination, especially if the spinal cord is compressed, impacting the signals to and from the brain.
What is cervical stenosis?
Cervical stenosis is the narrowing of the spinal canal in the neck, which can compress the spinal cord and nerves, causing pain, numbness, and weakness.
How can ergonomic adjustments at work help the cervical spine?
Ergonomic adjustments, such as proper chair height, monitor placement, and keyboard positioning, can reduce strain on the neck, preventing pain and long-term cervical spine issues.
What are some non-surgical treatments for cervical spine issues?
Non-surgical treatments include physical therapy, medications (pain relievers, anti-inflammatory drugs), cervical traction, heat/cold therapy, and lifestyle modifications.
How do spinal nerves exit the cervical spine?
Spinal nerves exit the cervical spine through openings called intervertebral foramina, located between adjacent vertebrae, to innervate various parts of the body.
Can sports injuries affect the cervical spine?
Yes, sports injuries can lead to acute cervical spine issues such as fractures, dislocations, and soft tissue injuries, requiring prompt medical attention.
How important is neck muscle strength for cervical spine health?
Strong neck muscles provide crucial support to the cervical spine, help maintain proper posture, and prevent injuries by absorbing and distributing forces during movement.
What is the cervical lordosis, and why is it important?
Cervical lordosis refers to the natural inward curve of the cervical spine, essential for proper alignment, balance, and shock absorption.
Can cervical spine problems cause symptoms in other parts of the body?
Yes, cervical spine problems can cause referred pain, numbness, or weakness in the shoulders, arms, and hands due to nerve compression or irritation.
What role do chiropractors play in managing cervical spine issues?
Chiropractors can provide non-invasive treatments such as spinal adjustments, mobilizations, and therapeutic exercises to help manage and alleviate cervical spine issues. However, it is important to consult with a medical doctor before starting any new treatment.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

