Cervical Spine Surgery
If cervical spine pain becomes severe enough to disrupt daily activities or is accompanied by swelling, tenderness, or redness, seeking medical attention is essential.
At Complete Orthopedics, our skilled cervical spine specialists excel in treating cervical spine pain using both surgical and non-surgical methods. We evaluate symptoms, identify the problem, and suggest suitable treatments, including surgery if necessary.
We cater to New York City and Long Island and work with six hospitals, offering state-of-the-art cervical spine surgery and comprehensive orthopedic services. Consultations with our orthopedic surgeons can be scheduled online or by phone.
Learn about common causes of cervical spine pain and the treatment options available, including when surgery is the best choice.
Overview
Patients who have failed conservative treatment for their cervical spine disease or patients who have sudden onset or worsening of their neurological symptoms, may need to undergo cervical spine surgery. Cervical spine surgery is usually done from the front or the back of the neck.
It involves decompression of the nerves or the spinal cord as dictated by the pathology. These patients have usually undergone prior advanced imaging to confirm their diagnosis. Patients with emergency deterioration or new onset motor weakness or bowel or bladder or gait involvement may need cervical spine surgery on an emergent or urgent basis.
Rest of the patients have usually tried conservative means with no or little benefit. Surgery done from the front of the neck, usually involves removal of the disc material with placement of a cage between the two vertebrae and a plate in front. It can be done on one or more than one levels as required.
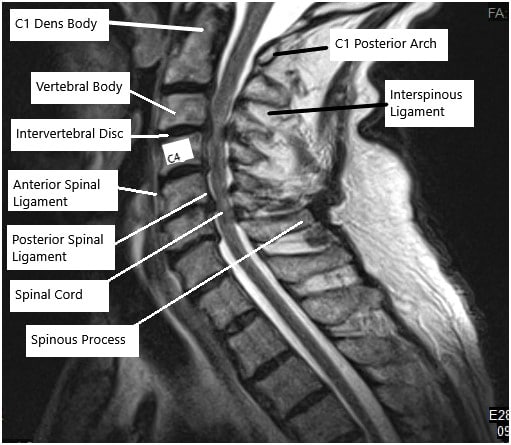
MRI of the cervical spine
Patients who have compression from the back of the vertebra may need surgery from the back in which the lamina is removed and the spinal cord and the nerve roots are decompressed. This is usually combined with fusion using screws and rods.
Occasionally, the patient may be a good candidate for motion sparing surgery like Microdiscectomy or Laminoplasty. When indicated, patients may be a good candidate for cervical disc replacement in which the disc from the front of the vertebrae are removed and replaced with the artificial disc.
This surgery allows retention of the mobility between the vertebrae and results in preservation of the neck motion after the surgery. All cervical spine surgeries are performed under general anesthesia after endotracheal intubation.
Cervical Microdiscectomy
This is a minimal invasive procedure which is usually done in carefully selected patients to remove the pressure of the disc over the nerve root causing the pain. This surgery is done from the back of the neck in which a limited amount of bone is removed to form a window to decompress the nerve root and remove the bulging disc material. This surgery allows retention of movement between the vertebrae as there is no fusion involved. The recovery and rehabilitation from this surgery is faster and has good results.
Cervical Laminectomy
Cervical laminectomy is the procedure of removal of the lamina or the bone on the back of the vertebrae of the neck. This procedure is usually done for patients who have compression of the spinal cord from the back or patients who have narrowing of the spinal canal at multiple levels. This surgery is combined with fusion of the neck from the back using screws and rods. The patients usually have to use a neck collar for a few weeks and there is a gradual recovery over a span of two to three months. The patients usually will have some restriction of movement after the surgery, especially if it is performed at multiple levels.
Cervical Laminoplasty
Laminoplasty is a motion sparing surgery that is performed over multiple levels on the back of the neck. This surgery is usually performed in stable spine. Window is made on the lamina of the cervical vertebrae and this window is held open with use of mini plates. This surgery is performed in patients who have narrowing of the spinal canal at multiple levels, especially from the back side. This surgery allows retention of movements of the neck as oppose to laminectomy and fusion surgery in which there is some restriction of movements. The patients usually must wear a neck collar for a couple of weeks and there is a gradual recovery over a span of two to three months.
Anterior Cervical Discectomy and Fusion
ACDF is one of the most common surgical procedure performed over the cervical spine. It is usually performed for degenerative disc disease of the neck along with disc herniation causing compression on the spinal cord or nerve roots. It is also performed in cases of fracture or dislocation of the spine. This surgery is performed from the front of the neck in which the disc is removed and is replaced with cage along with autograft and the two vertebrae are fixed to each other with use of plate and screws. It can be performed at one or more than one levels as required. The success rate of the surgery is very good, and patients have a gradual recovery over a span of six to eight weeks.

Rigid distraction forceps
The rigid distraction forceps in the image above are used to create space between the diseased cervical vertebrae to remove the disc material and subsequent insertion of bone cage.

ACDF plate
The image above shows a plate used to fuse the cervical vertebrae in anterior cervical decompression and fusion surgery. The surgery is performed from the front of the neck and a plate is fixed with the help of screws.
Anterior Cervical Corpectomy and Fusion
ACCF is another form of surgery on the neck from the front in which the body of one or more than one vertebra are removed and replaced with cage with or without bone graft along with fixation of the spine using plate and screws. This surgery is usually performed if there is compression at multiple levels or especially behind the vertebral body which cannot be removed by doing a simple discectomy as in ACDF. The recovery from this surgery is slower than ACDF and the patient may require wearing a brace for a longer period.
Total Disc Replacement
Total disc replacement of cervical spine is an excellent procedure done in well selected candidates. As opposed to fusion, TDR helps in retaining the movements of the cervical spine and at the same time taking care of the degenerated disc and removing the pressure over the spinal cord or nerve roots. Total disc replacement can be usually performed at one or two levels and helps preventing the problems associated with fusion surgery. Total disc replacement is contraindicated in patients with instability or infection of the cervical vertebrae, tumors, osteoporosis.

Total Cervical Disc Replacement and parts of cervical vertebrae (anterior view)
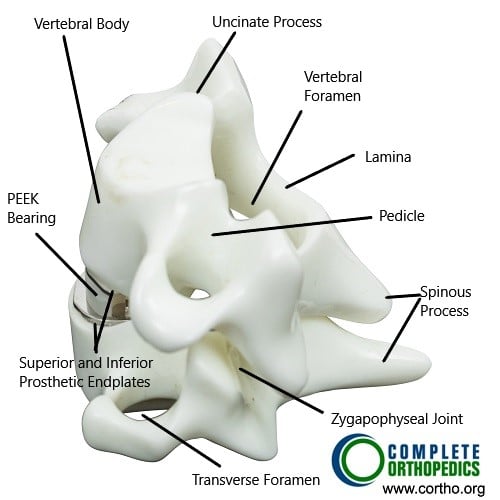
Total Cervical Disc Replacement and parts of cervical vertebrae (lateral view)
The images above show a total cervical disc replacement along with various parts of the cervical vertebrae. The PEEK (poly ether-ether ketone) polymer is used as a bearing surface. The prosthetic replaced disc re-duplicated the function of the normal cervical intervertebral disc.
Preoperative Workup
The patients are usually seen by the physician and appropriate preoperative investigations including advanced imaging, blood work and ECG and chest x-rays as needed are done. The patients may also need clearance from their primary care physician and anesthesiologist before the surgery. The patients are instructed to come to the hospital two hours in advance with no jewelry. The patients are taken to the preoperative area where they are seen by the anesthesiologist and appropriate procedure performed before the patient is taken to the operating room. In the operating room the patient usually is given general anesthesia and intubated before being positioned for the surgery.
Postoperative Care And Recovery After Cervical Spine Surgery
The patients who undergo cervical spine surgery are usually extubated after the surgery and some patients who undergo surgeries like ACDF can be discharged home on the same day if they meet the criteria to discharge. Most of the time cervical spine surgery patients are admitted to the hospital for one to five days depending on the surgery and recovery. Patients can mobilize in and out of bed with or without a neck collar or support depending on the surgery and recovery from anesthesia.
Immediately after the surgery, the patients are encouraged to do their activities of daily living from the first postop day. The patients are provided with medications in the hospital as well as for home to take care of pain and muscle spasms that can develop after the surgery. Incisions need to be kept clean and dry. The patients are instructed to avoid bath and hot tubs, swimming, heavy lifting, driving and smoking. The patients can take shower and remove the dressings after 72 hours from surgery and replace it with dry dressing. The patients are advised to eat healthy and nutritious diet with lot of fibers. The patients are also instructed to use over-the-counter laxatives for constipation that may develop due to pain medications.
Risks And Complications
As for all surgeries there are certain but rare risks for anesthesia including cardiac arrest, stroke, paralysis, and rarely death.
Risks of Cervical spine surgery may include though not limited to:
- Hematoma or hemorrhage
- Damage to the carotid or vertebral artery which may result in a stroke or excessive bleeding, even death
- Blindness
- Damage to the nerve in the neck resulting in hoarseness or swallowing difficulties
- Damage to the food or wind pipe
- Damage to the dura, resulting in a cerebrospinal fluid leak
- Failure, loosening or pull out of the graft, cage, implant or plate
- Wound infection
- Failure of fusion to happen
- Damage to the spinal cord or nerve root(s) resulting in new onset or deterioration of preexisting pain, weakness, paralysis, loss of sensation, loss of bowel or bladder function, impaired sexual function, etc., which may or may not recover.
- A few of these conditions may warrant repeat surgery
Certain patient population is at a higher risk for complication which include but are not limited to:
- Smoking
- Seizures
- Obstructive sleep apnea
- Obesity
- High blood pressure
- Diabetes
- Other medical conditions involving your heart, lungs or kidneys
- Medications, such as aspirin, that can increase bleeding
- History of heavy alcohol use
- Drug allergies
- History of adverse reactions to anesthesia
When To Visit An Emergency Room After A Surgery:
- Suspected cardiac problem: severe chest pain or pressure, shortness of breath, tightness in chest, pain in left arm, jaw pain, dizziness or fainting, unexplained weakness or fatigue, rapid or irregular pulse, sweating, cool, clammy skin, and/or paleness
- Suspected Stroke: trouble speaking, changes in vision, confusion or other change in mental status
- Suspected venous thrombosis: swelling of the legs, ankles, or feet, discomfort, heaviness, pain, aching, throbbing, itching, or warmth in the legs, sudden shortness of breath, chest pain, coughing up blood, rapid or irregular heart rate
- Suspected Sepsis: high grade fever, with shivers associated with fatigue, dizziness, racing heart, pale or discolored skin, sleepy, difficult to rouse, confused, short of breath
- Heavy bleeding from the surgical site
- Severe allergic reaction with trouble breathing, swelling, hives
When To Contact A Doctor’S Office After Surgery:
- temperature more than 101 degrees Fahrenheit
- increased pain or tenderness near the incision
- poor pain relief
- signs of infection: increased swelling, redness, increased drainage, increased warmth, pus, foul smell, bleeding at the incision, incision coming apart
- increased numbness, numbness in genital area
- inability to feel or move fingers or toes
- pale blue, white or abnormally cold fingers or toes
- nausea (upset stomach) or vomiting (throwing up) that won’t stop
- increased tiredness
- a generally worse feeling than you had when you left the hospital
- problems urinating, severe constipation or severe diarrhea
- a concern about any other symptoms that seem unusual
Do you have more questions?
What types of cervical spine surgery are there?
The main types include anterior cervical discectomy and fusion (ACDF), anterior cervical corpectomy and fusion (ACCF), cervical microdiscectomy, cervical laminectomy, cervical laminoplasty, and total disc replacement (TDR).
What are the main reasons for needing cervical spine surgery?
Cervical spine surgery is needed if conservative treatments fail or if there is a sudden onset or worsening of neurological symptoms, such as motor weakness, bowel or bladder issues, or gait problems.
What is the difference between surgery performed from the front and the back of the neck?
Front (anterior) surgery usually involves removing disc material and placing a cage and plate, while back (posterior) surgery often involves removing the lamina and decompressing the spinal cord and nerve roots, often combined with fusion using screws and rods.
What is an anterior cervical discectomy and fusion (ACDF)?
ACDF involves removing a diseased disc from the front of the neck and replacing it with a cage and bone graft, then fixing the vertebrae with a plate and screws.
What is a cervical microdiscectomy?
It is a minimally invasive procedure to remove pressure from the disc on the nerve root, done from the back of the neck, allowing movement between vertebrae since no fusion is involved.
What are the benefits of total disc replacement (TDR)?
TDR retains movement in the cervical spine and alleviates pressure on the spinal cord or nerve roots, avoiding the issues associated with fusion.
What preoperative workup is needed before cervical spine surgery?
Patients undergo advanced imaging, blood work, ECG, and chest x-rays. They may also need clearance from their primary care physician and anesthesiologist.
What does postoperative care and recovery involve?
Recovery includes hospital stay of one to five days, activity encouragement from the first day post-op, pain management, and instructions on wound care and activity restrictions.
What are the common risks and complications of cervical spine surgery?
Risks include hematoma, damage to arteries, nerve damage, CSF leaks, implant failure, infection, and spinal cord damage, among others.
What factors increase the risk of complications?
Higher risk factors include smoking, seizures, obstructive sleep apnea, obesity, high blood pressure, diabetes, other medical conditions, certain medications, heavy alcohol use, and drug allergies.
What should I avoid after cervical spine surgery?
Avoid baths, hot tubs, swimming, heavy lifting, driving, and smoking. Follow specific guidelines for showering and wound care.
How long will I need to wear a neck collar after surgery?
The duration varies depending on the surgery but typically ranges from a couple of weeks to a few months.
What symptoms warrant an immediate visit to the emergency room post-surgery?
Symptoms include severe chest pain, shortness of breath, confusion, swelling in the legs, high fever, heavy bleeding, and severe allergic reactions.
When should I contact my doctor’s office after surgery?
Contact your doctor if you have a fever over 101°F, increased pain, signs of infection, increased numbness, difficulty urinating, severe constipation, or any concerning symptoms.
What activities can I do immediately after surgery?
Patients are encouraged to perform their daily activities from the first day post-op as tolerated, with specific instructions from their healthcare provider.
How long does it take to recover from cervical spine surgery?
Recovery varies by surgery type, ranging from six to eight weeks for procedures like ACDF to a few months for more extensive surgeries.
Can cervical spine surgery be done as an outpatient procedure?
Yes, some surgeries like ACDF may allow for same-day discharge if the patient meets specific criteria.
What is a cervical laminoplasty?
A motion-sparing surgery that involves creating a window in the lamina and holding it open with mini plates, preserving neck movements.
What is a cervical laminectomy?
It involves removing the lamina to decompress the spinal cord, often combined with fusion using screws and rods, leading to some movement restriction.
How is cervical spine surgery performed under anesthesia?
It is performed under general anesthesia with endotracheal intubation to ensure the patient is unconscious and pain-free during the procedure.
What is the purpose of fusion in cervical spine surgery?
Fusion stabilizes the spine by joining two or more vertebrae, which is necessary when decompression alone is insufficient.
What is the role of advanced imaging in cervical spine surgery?
Advanced imaging, such as MRI, helps confirm the diagnosis and plan the surgical approach by identifying the specific pathology.
Why might total disc replacement be contraindicated?
TDR is not suitable for patients with spine instability, infection, tumors, or osteoporosis.
What are the indications for cervical spine surgery on an emergent basis?
Emergency indications include new onset motor weakness, bowel or bladder dysfunction, and significant gait disturbances.
What kind of postoperative medication can I expect?
Medications for pain and muscle spasms, and possibly over-the-counter laxatives to counteract constipation from pain medications.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

