Cervical Spine Stenosis
Cervical spine discomfort affects many individuals, but if it becomes more severe and starts impacting your daily activities, or if it’s accompanied by swelling, tenderness, or inflammation, it’s essential to seek medical attention.
Situated in New York City and Long Island, we have access to six hospitals and modern facilities for advanced cervical spine surgeries and orthopedic care. Scheduling a consultation with an orthopedic surgeon is simple—either online or by phone.
Discover the various causes and treatments for cervical spine pain, and understand when surgery is the most appropriate option.
Overview
Cervical spinal stenosis is the narrowing of the spaces in the cervical spine leading to compression of the nerves or the spinal cord.
The narrowing is usually caused by age-related wear and tear of the structures of the cervical vertebral column, usually affecting patients aged 50 years and more. The patients commonly complain of neck pain but may also complain of symptoms such as numbness and tingling of the arms.
The cervical vertebral column extends from the base of the skull to the upper chest. Apart from providing stability and aiding in the movement of the head, the cervical vertebral column creates a central canal that provides a safe conduit for the spinal cord to travel from the brain down the body.
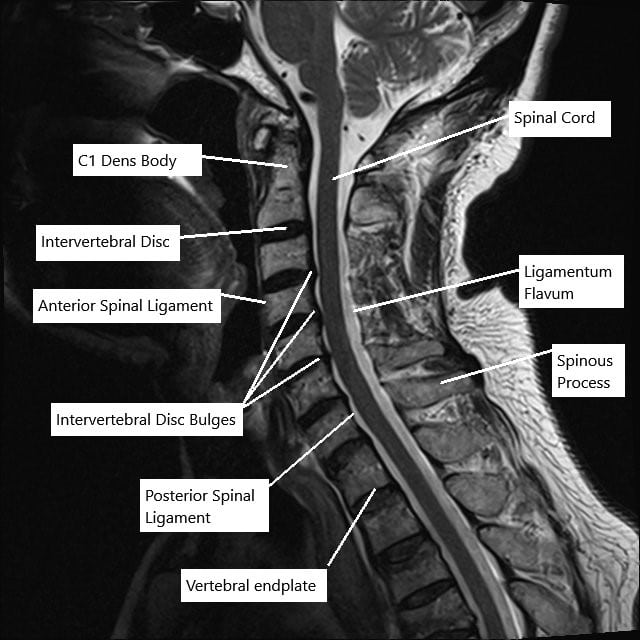
MRI of the cervical spine in sagittal section showing disc herniations.
The spinal cord carries the nerve transmissions from the brain and helps in moving the body, relaying the sensations from various parts, and coordinating the activities of different organ systems and limbs.
The spinal cord gives numerous branches as it descends down the central canal known as nerve roots which unite to form different nerves of the body. The nerves branch out through the intervertebral foramen created by two vertebrae stacked on each other.
Cervical Spinal Stenosis Causes
The cervical spine stenosis results from compression from the spinal cord or the nerve roots as they pass through the cervical vertebral column. The most common cause is the wear and tear arthritis of the cervical spine in the elderly population.
The arthritis of the cervical spine may lead to the formation of bone spurs known as osteophytes. The osteophytes may arise from the facet joint or the vertebral body and may compress the neural structures.
Spondylolisthesis is a condition where the vertebrae are not aligned properly over one another. The malalignment of the vertebrae may compress the spinal cord or the nerve roots leading to cervical spinal stenosis.
The intervertebral disk is tissue present between two adjoining vertebrae that cushion the spine and provides stability to the spine. The soft gel-like interior part of the intervertebral disk may at times herniate through the outer annulus fibrosis.
The herniated disk in the cervical spine may narrow the space for the spinal cord or the nerve roots causing spinal stenosis.
Ligamentum flavum is a thick band of tissue present behind the spinal cord inside the central canal. Any thickening or buckling of the ligamentum flavum may cause significant narrowing of the canal leading to stenosis.
In some patients, the neural canal may be narrower by birth. These patients are particularly vulnerable to cervical spinal stenosis due to any pathological condition leading to further narrowing.
Some genetic conditions like osteopetrosis, Paget’s disease, or achondroplasia may also lead to cervical spinal stenosis. Other diseases implicated in spinal stenosis are acromegaly, ankylosing spondylitis, and fluorosis.
Other causes of cervical spinal stenosis include any injuries to the cervical spine causing collapse or dislocation of the vertebrae or displacement of the fragment inside the canal. All of which may cause narrowing of the space available for nervous tissue.
Location
Depending upon the location of the narrowing in the vertebra, the spinal stenosis may be classified as central, lateral, or foraminal. The central stenosis may be caused by posterior disk herniation, vertebral bone spurs, or buckling of the ligaments of the canal.
Lateral recess stenosis is usually a result of facet bone spurs. The far lateral or foraminal stenosis may result from a disk herniation in the foramen or malalignment of the vertebrae.
Pathology of age-related cervical spinal stenosis
With increasing age, the content of the tissue forming the intervertebral disk changes leading to small tears in the disk. This leads to loss of disk height and building of the disk and the posterior longitudinal ligament into the central canal.
This may cause buckling of the ligamentum flavum and subsidence of the facet joints. The facet joints try to restabilize the spine by forming new bone leading to bone spurs which may impinge upon the neural structures from behind.
The bone spurs formed from the vertebral body endplate may compress the neural structures from the front.
Cervical Spinal Stenosis Symptoms
Patients commonly report symptoms of neck pain and pain in both arms. The neck pain may be described as shooting down the arms or electrical sensations in the arms.
Cervical spinal stenosis may also result in a sensation of numbness and tingling in one or both the arms. In cases of a single nerve compression known as radiculopathy, the symptoms may be present only in the distribution of the involved nerve.
In advanced cases, as the disease progresses, patients may complain of the clumpiness of the hands and arms due to weakness and loss of coordination. In some cases of advanced stenosis, there may be loss of bowel bladder control and weakness of the feet and legs.
Cervical Spinal Stenosis Diagnosis
The condition is usually diagnosed by the orthopedic surgeon on physical examination after eliciting an elaborate history of the symptoms.
The physician may perform physical examinations to test for the integrity of the nervous system in all four limbs and certain reflexes. The physician may also move the patient’s neck to elicit pain and symptoms.
All the physical examination tests are directed to localize the level of compression in the cervical spine.
An X-ray is usually the first investigation of choice to look for bony abnormalities in the cervical spine. A CT scan often reveals more detail of the bony structures compared to an X-ray.
The various soft tissue and nervous structures are made visible on an MRI, through which the physician can localize the level of stenosis. An MRI also aids in planning any surgery needed to relieve the symptom of stenosis if needed.
Treatment
The treatment of cervical spinal stenosis is usually conservative/non-surgical. Conservative treatment includes physical therapy, pain relief medication, and cold/heat therapy.
Cortisone injections may be given through caudal, interlaminar, or transforaminal route. The cortisone injections provide symptomatic relief by reducing inflammation associated with stenosis.
Surgical management usually involves creating more space for the neural structures. Laminotomy involves the removal of part of the lamina (roof of the vertebrae) to create more space.
Laminectomy involves removal of the lamina which is often combined with additional measures to stabilize the spine. The vertebral opening for the nerves branching out may be widened by a procedure known as a foraminotomy. During the surgery, herniated disks and bone spurs may also be removed to create more space in the canal.
Laminoplasty is a procedure in which a hinge is created without removal of bone tissue and the canal is widened. The widened canal may be fixed with wires or special threads.
In cases of multiple level stenosis or when any procedure may result in instability of the spine, cervical spine surgery is performed from the front which is often combined with the fusion of two or more vertebrae.

Rasp used in ACDF

ACDF Plate with screws
The images above show a rasp used during the anterior decompression and fusion surgery. The rasp is used to prepare the end plate for insertion of bone cage and subsequent fixation of the vertebrae using the plate shown above.
Managing Life with Cervical Spinal Stenosis
Living with cervical spinal stenosis can be challenging, but there are ways to manage the condition and maintain a good quality of life:
- Stay Active: Engage in low-impact exercises like walking or swimming to keep your spine flexible.
- Use Good Posture: Maintain proper posture to reduce strain on your neck.
- Avoid Heavy Lifting: Prevent further strain on your spine by avoiding heavy lifting or bending activities.
- Healthy Diet: A balanced diet rich in calcium and vitamin D can help maintain bone health.
- Ergonomic Adjustments: Make adjustments to your work and home environments to reduce strain on your neck.
When to See a Doctor
It’s important to seek medical attention if you experience:
- Severe neck pain that doesn’t improve with rest.
- Numbness or weakness that affects your daily activities.
- Loss of bladder or bowel control.
- Difficulty walking or maintaining balance.
Early diagnosis and treatment can help prevent the progression of cervical spinal stenosis and improve your overall quality of life.
Conclusion
Cervical spinal stenosis is a manageable condition with a variety of treatment options available. Understanding the causes, symptoms, and treatment options can help you make informed decisions about your health. Always consult with a healthcare professional for a diagnosis and personalized treatment plan.
Do you have more questions?
Can cervical spinal stenosis be completely cured?
While cervical spinal stenosis cannot be completely cured, symptoms can be managed effectively with a combination of non-surgical and surgical treatments depending on the severity of the condition.
Are there any activities that should be avoided with cervical spinal stenosis?
Activities that put excessive strain on the neck, such as heavy lifting, high-impact sports, and certain exercises, should be avoided to prevent exacerbation of symptoms.
How long does it take to recover from surgery for cervical spinal stenosis?
Recovery time can vary, but generally, patients may need several weeks to a few months to recover from cervical spine surgery, with physical therapy playing a crucial role in the rehabilitation process.
Is physical therapy always required after surgery for cervical spinal stenosis?
Yes, physical therapy is typically recommended after surgery to help restore mobility, strengthen muscles, and ensure proper healing.
Can cervical spinal stenosis cause headaches?
Yes, cervical spinal stenosis can sometimes cause headaches, particularly if the stenosis affects the upper cervical vertebrae.
Are there any long-term effects of cervical spinal stenosis on daily life?
Long-term effects can include chronic pain, reduced mobility, and in severe cases, neurological deficits. However, with proper treatment, many people can manage their symptoms and maintain a good quality of life.
How is cervical spinal stenosis different from lumbar spinal stenosis?
Cervical spinal stenosis affects the neck region of the spine, while lumbar spinal stenosis affects the lower back. Symptoms and potential complications differ based on the location of the stenosis.
Can lifestyle changes help manage cervical spinal stenosis symptoms?
Yes, maintaining a healthy weight, regular low-impact exercise, good posture, and ergonomic adjustments at work can help manage symptoms.
What is the success rate of surgery for cervical spinal stenosis?
Surgery for cervical spinal stenosis has a high success rate, with many patients experiencing significant relief from symptoms. Success rates can range from 70% to 90%, depending on the procedure and patient condition.
Can cervical spinal stenosis lead to paralysis?
In severe cases where the spinal cord is significantly compressed, cervical spinal stenosis can lead to paralysis, but this is relatively rare with early and appropriate treatment.
Are there any non-pharmacological treatments for pain management in cervical spinal stenosis?
Yes, non-pharmacological treatments include physical therapy, acupuncture, chiropractic care, and cognitive-behavioral therapy for pain management.
What role does genetics play in cervical spinal stenosis?
Genetics can play a role, particularly if there is a family history of spinal conditions or congenital spinal canal narrowing.
Is there a way to prevent cervical spinal stenosis?
While you cannot prevent the aging process, you can reduce the risk by maintaining a healthy lifestyle, avoiding neck injuries, and managing underlying conditions like arthritis.
Can cervical spinal stenosis cause sleep problems?
Yes, pain and discomfort from cervical spinal stenosis can interfere with sleep, making it difficult to find a comfortable position.
How often should someone with cervical spinal stenosis see a doctor?
Regular follow-ups every six months to a year, or more frequently if symptoms worsen, are recommended to monitor the condition and adjust treatment as needed.
Are there any alternative therapies that can help with cervical spinal stenosis?
Alternative therapies such as acupuncture, yoga, massage, and herbal supplements may provide symptom relief for some individuals, but should be discussed with a healthcare provider.
Can cervical spinal stenosis cause dizziness or vertigo?
Yes, cervical spinal stenosis can sometimes cause dizziness or vertigo, particularly if the blood flow to the brain is affected.
What imaging tests are best for diagnosing cervical spinal stenosis?
MRI is the most effective imaging test for diagnosing cervical spinal stenosis as it provides detailed images of the spinal cord and nerves. CT scans and X-rays are also useful.
What is the difference between myelopathy and radiculopathy in cervical spinal stenosis?
Myelopathy refers to spinal cord compression causing symptoms like difficulty walking and fine motor problems, while radiculopathy involves nerve root compression, leading to pain, numbness, and weakness in the arms.
Can cervical spinal stenosis cause problems with swallowing?
In rare cases, severe cervical spinal stenosis can cause problems with swallowing if the spinal cord compression affects the nerves that control the throat muscles.
What medications are commonly prescribed for cervical spinal stenosis?
Common medications include nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, pain relievers, and sometimes corticosteroids to reduce inflammation.
How does cervical spinal stenosis affect mobility?
It can affect mobility by causing pain, stiffness, and muscle weakness, which can make it difficult to perform daily activities and maintain balance.
What should I do if I suspect I have cervical spinal stenosis?
If you suspect you have cervical spinal stenosis, it is important to see a healthcare provider for an evaluation. Early diagnosis and treatment can help manage symptoms and prevent complications.
What is the most common age for developing cervical spinal stenosis?
Cervical spinal stenosis is most commonly seen in people over the age of 50, as it is often related to degenerative changes in the spine that occur with aging.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

