Medial Patellofemoral Ligament Reconstruction
When knee discomfort escalates, hindering daily tasks, or presents swelling, tenderness, or inflammation, it’s imperative to seek medical attention. At Complete Orthopedics, our specialized team concentrates on addressing knee bursitis through tailored strategies and surgical interventions. We prioritize comprehending symptoms, pinpointing issues, and proposing appropriate treatments or surgeries.
With branches in New York City and Long Island, and affiliation with six hospitals, we provide cutting-edge facilities for advanced knee care. Arrange a consultation with an orthopedic surgeon conveniently via our online platform or by phone. Educate yourself about the causes and remedies for knee discomfort, and discern when surgery emerges as the optimal solution.
Overview
The medial patellofemoral ligament (MPFL) is a tough structure present on the inner side of the knee. The ligament connects the undersurface of the kneecap to the inner side of the lower thigh bone. Damage to the medial patellofemoral ligament may result in instability of the kneecap resulting in recurrent dislocations.
The kneecap (patella) sits in a groove in front of the knee formed by the lower end of the thigh bone. The patella attaches the thigh-muscle tendon to the front of the shin bone. The kneecap moves to form the joint with the thigh bone, resulting in smooth bending and straightening of the knee.
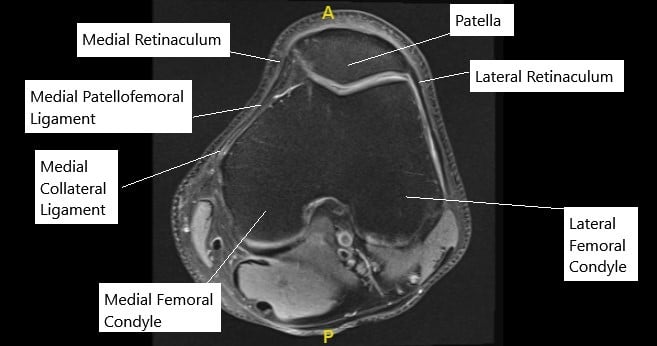
MRI of the knee in axial section showing normal MPFL.
During the motion of the kneecap, medial patellofemoral ligament aids to keep the kneecap in place acting as a leash. Traumatic injuries and athletic activities may result in patellar dislocation which is usually towards the outer side. The medial patellofemoral ligament is usually torn in the process.
Symptoms of Medial Patellofemoral Ligament (MPFL) injury
Medial Patellofemoral Ligament (MPFL) injury typically presents with several distinctive symptoms that can vary in intensity depending on the severity of the injury. The MPFL is a crucial ligament that stabilizes the patella (kneecap) and prevents it from dislocating towards the outer side of the knee. When this ligament is injured, it can lead to significant discomfort and functional limitations. Here are the common symptoms associated with MPFL injury:
Pain: Pain is usually the first symptom experienced with an MPFL injury. It can be localized to the inner side of the knee or around the patella. The pain may range from mild to severe and can be aggravated by activities that involve bending or straightening the knee, such as walking, running, or climbing stairs.
Swelling: Swelling around the patella or throughout the knee joint is another typical symptom of MPFL injury. The swelling may develop rapidly after the injury or gradually over time and can contribute to stiffness and limited range of motion in the knee.
Instability or Feeling of Giving Way: Since the MPFL plays a crucial role in stabilizing the patella, its injury can lead to a sense of instability in the knee. Patients may describe a feeling of the knee “giving way” or feeling as though it might dislocate, especially during activities that require sudden changes in direction or weight-bearing.
Difficulty Straightening the Knee: In some cases, individuals with an MPFL injury may experience difficulty fully straightening the affected knee. This limitation in extension, also known as knee flexion contracture, can further contribute to functional impairment and discomfort.
Audible Popping or Clicking Sensation: Injuries to the MPFL can sometimes be accompanied by audible popping or clicking sensations within the knee joint, particularly during movement. These sounds may occur due to the patella shifting out of its normal alignment or rubbing against other structures within the knee.
Tenderness to Touch: The area around the inner side of the knee, where the MPFL attaches to the femur and patella, may become tender to the touch. Palpating this area can elicit pain and discomfort, especially if the injury is acute or if there is associated inflammation.
Causes of MPFL Injury:
Direct Trauma: A significant blow or impact to the knee, such as a fall or collision during sports activities, can result in MPFL injury. This trauma may cause stretching or tearing of the ligament.
Repetitive Stress: Activities that involve repetitive bending, twisting, or sudden changes in direction can put excessive stress on the MPFL, leading to gradual wear and tear over time. This is particularly common in athletes who participate in sports like basketball, soccer, or volleyball.
Genetic Factors: Some individuals may have an inherent predisposition to ligament laxity or abnormalities in the alignment of the patella and femur, increasing their risk of MPFL injury.
Muscular Imbalance: Weakness or imbalance in the muscles surrounding the knee, especially the quadriceps and hamstrings, can disrupt the normal function of the MPFL and contribute to its injury.
Besides traumatic injuries or athletic injuries, some patients may be prone to kneecap dislocation owing to the increased laxity in their joints and ligaments, or due to tight structures (patellar retinaculum) on the outer side of the knee joint.
The torn ligament may heal naturally but usually heals in a slack manner causing instability of the kneecap. This may result in recurrent instability further aggravating the condition. Further, over time, the cartilage forming the patellofemoral joint may wear out leading to arthritis and degenerative changes.
Diagnosis
The physician may diagnose the torn MPFL after eliciting a history of the pattern of injury, prior history of dislocations, and a thorough physical examination. The physical examination may include provocative tests to look for patellar mal-tracking and instability.
The physician may request radiological studies in the form of X-rays, CT scans to look for instability and malalignment of the extremity. Using an MRI the physician is able to clearly discern the various soft tissues including the MPFL of the knee joint.
Treatment
Patients with two or more kneecap dislocations may be offered surgical management. Surgical management may also be offered to patients with a single episode of kneecap dislocation who may need surgery for other knee disorders. The MPFL reconstruction surgery may be safely offered in children and adults alike.
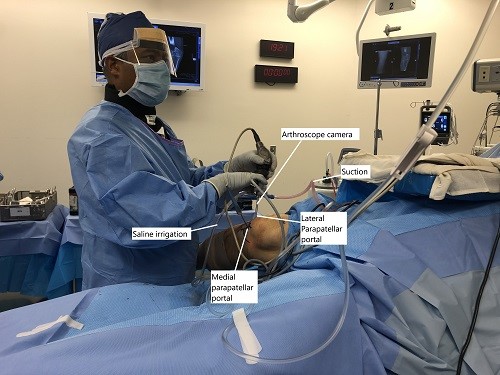
Intraoperative image showing arthroscopic repair of MPFL.
General or regional anesthesia in the form of spinal anesthesia may be used in MPFL reconstruction surgery. In general anesthesia, the patient sleeps during the surgery with the relaxation of all the muscles of the body. In spinal anesthesia, only the lower extremities are numb and relaxed, the patient is usually awake but maybe sedated to help the patient sleep.
The MPFL reconstruction surgery involves the use of a tendon graft to reconstruct the MPFL. The surgery is performed with the help of an arthroscope. Arthroscopic surgery involves the use of tiny (<1cm) incisions. Through the incisions, a tiny camera with a light source is inserted that displays live images on an external monitor.
Tiny minuscule instruments are inserted through another small incision and the surgeon uses the instruments to complete the surgery. The surgeon first uses the instruments to cut and release the tight patellar retinaculum on the outer side of the knee.
A tendon graft (semitendinosus) is harvested from one of the hamstring muscles. The tendon graft is then shaped to insert one end at the inner side of the kneecap. The other end is inserted at the inner side of the femoral condyle. The ends are secured using screws at both ends.
In patients with patellar maltracking due to mal-alignment of the bones, a tibial tuberosity osteotomy may be done. The osteotomy involves the placement of the tuberosity towards the inner side of the knee. The MPFL reconstruction surgery may also be performed in patients who have had prior surgeries in the form of debridement, or release of the retinaculum for kneecap instability.
The patient’s knee is placed in a brace after the surgery. The brace helps to keep the knee straight while walking and activities of daily living. Some pain and swelling are normal after the surgery and the patient may be prescribed pain medications. The patients are also advised regular icing and leg elevation to reduce postoperative swelling.
Recovery and Rehabilitation
Recovery from MPFL Reconstruction typically involves a period of rest followed by physical therapy. During this time, you’ll work on regaining strength and mobility in your knee. Your healthcare team will provide guidance on exercises and activities to help you recover safely and effectively.
It’s important to follow your doctor’s instructions carefully during this time to ensure proper healing and minimize the risk of complications. While recovery can vary from person to person, most individuals can expect to return to their normal activities within a few months of surgery.
Benefits of MPFL Reconstruction
MPFL Reconstruction offers several benefits for individuals experiencing knee instability:
Improved Stability: By repairing the MPFL, the surgery helps restore stability to the knee joint, reducing the risk of patellar dislocations.
Pain Relief: For many people, MPFL Reconstruction can alleviate pain and discomfort associated with knee instability.
Enhanced Function: With a stable knee joint, you’ll likely experience improved function and mobility, allowing you to participate in activities without fear of injury.
Risks and Considerations:
Like any surgery, MPFL Reconstruction carries some risks and considerations. These may include:
Infection: There is a small risk of infection at the surgical site, which can usually be managed with antibiotics.
Graft Failure: In some cases, the graft used in MPFL Reconstruction may fail to properly integrate with the surrounding tissue, requiring additional surgery.
Limited Range of Motion: You may experience temporary stiffness or limited range of motion in the knee following surgery, though this typically improves with time and physical therapy.
Do you have more questions?
How long does the surgery typically take?
The surgery usually takes about 1 to 2 hours to complete, depending on the complexity of the case.
Is MPFL Reconstruction performed under general anesthesia?
Yes, MPFL Reconstruction is typically performed under general anesthesia to ensure patient comfort throughout the procedure.
Will I need to stay in the hospital overnight after surgery?
In most cases, MPFL Reconstruction is performed as an outpatient procedure, meaning you can go home the same day. However, your surgeon will determine if overnight observation is necessary based on your individual circumstances.
How soon after surgery can I return to work or school?
The timing of your return to work or school will depend on the type of job or activities you engage in. In general, most patients can resume light activities within a few days to a week after surgery, but more strenuous activities may need to be avoided for several weeks.
What type of physical therapy will I need after MPFL Reconstruction?
Your physical therapy program will be tailored to your specific needs and goals, but it typically involves exercises to improve strength, flexibility, and range of motion in the knee. Your therapist will guide you through the process and monitor your progress closely.
How long will it take to fully recover from MPFL Reconstruction?
Recovery time can vary depending on factors such as the extent of the injury, the type of surgery performed, and individual healing rates. In general, most patients can expect to return to normal activities within 3 to 6 months after surgery.
Will I need to wear a brace after MPFL Reconstruction?
Your surgeon may recommend wearing a knee brace for a period of time after surgery to provide added support and stability to the knee joint during the initial stages of healing. However, this will depend on your specific situation and will be discussed with you before and after surgery.
What are the potential complications of MPFL Reconstruction?
Complications from MPFL Reconstruction are rare but can include infection, graft failure, stiffness, and nerve damage. Your surgeon will discuss these risks with you in detail before surgery and take steps to minimize them during the procedure.
How soon after surgery can I resume sports or physical activities?
You will need to wait until your surgeon and physical therapist determine that it is safe for you to return to sports or physical activities. This typically occurs around 4 to 6 months after surgery, although the timing may vary depending on your progress and the type of activities you wish to resume.
Will I be able to kneel after MPFL Reconstruction?
Most patients are able to kneel comfortably after MPFL Reconstruction once they have fully healed and completed their physical therapy program. Your surgeon will provide guidance on when it is safe to resume kneeling activities.
Can MPFL Reconstruction be performed using minimally invasive techniques?
Yes, MPFL Reconstruction can often be performed using minimally invasive techniques, which can result in smaller incisions, less pain, and faster recovery times compared to traditional open surgery.
How successful is MPFL Reconstruction in preventing future dislocations?
MPFL Reconstruction is generally highly successful in preventing future patellar dislocations, with success rates ranging from 85% to 95%. However, individual results may vary, and factors such as compliance with rehabilitation and activity modification can impact outcomes.
Will I need to avoid certain activities after MPFL Reconstruction?
Your surgeon may recommend avoiding high-impact activities or sports that involve repetitive twisting or pivoting movements to reduce the risk of reinjury to the knee. Your specific activity restrictions will be discussed with you during your postoperative appointments.
Can MPFL Reconstruction be performed as a standalone procedure, or is it typically done in conjunction with other knee surgeries?
MPFL Reconstruction can be performed as a standalone procedure or as part of a larger knee stabilization surgery, depending on the individual’s needs and the underlying cause of knee instability.
How soon after surgery will I be able to drive?
You should avoid driving until you are no longer taking prescription pain medication and can safely operate a vehicle. This typically occurs within a few days to a week after surgery, but you should check with your surgeon for specific guidance.
Will I need to undergo physical therapy before surgery?
Preoperative physical therapy may be recommended in some cases to help improve knee strength and range of motion prior to surgery. Your surgeon will advise you on whether prehabilitation is necessary based on your individual circumstances.
Are there any dietary restrictions I need to follow before or after surgery?
Your surgeon may recommend fasting for a certain period before surgery to reduce the risk of complications related to anesthesia. After surgery, it’s important to eat a healthy, balanced diet to support healing and recovery.
How long will I need to wear a knee brace after surgery?
The duration of knee brace use after surgery will vary depending on your surgeon’s recommendations and your individual progress. Some patients may only need to wear a brace for a few weeks, while others may require more extended use.
Will I need crutches after MPFL Reconstruction?
Crutches may be used immediately after surgery to help you move around safely while your knee heals. Your surgeon will advise you on how long you need to use crutches based on your specific situation.
Can MPFL Reconstruction be performed on both knees simultaneously?
While it is technically possible to perform MPFL Reconstruction on both knees at the same time, this approach is less common and may require a longer recovery period. Your surgeon will discuss the risks and benefits of bilateral surgery with you if it is deemed necessary.
How often will I need to follow up with my surgeon after MPFL Reconstruction?
You will typically have several follow-up appointments with your surgeon in the weeks and months following MPFL Reconstruction to monitor your progress, address any concerns, and adjust your treatment plan as needed.
Will I need to wear a brace during physical activity after I have fully recovered?
Your surgeon may recommend wearing a knee brace during high-risk activities or sports even after you have fully recovered from MPFL Reconstruction. This can provide added protection and reduce the risk of reinjury to the knee.
Can MPFL Reconstruction be performed on children or adolescents?
MPFL Reconstruction can be performed on children or adolescents who have persistent knee instability and recurrent patellar dislocations that have not responded to conservative treatment. However, the decision to proceed with surgery in this population should be carefully considered and discussed with a pediatric orthopedic specialist.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

