Exercises After Hip Replacement
Exercises after hip replacement surgery form an important part of the recovery and rehabilitation process. The success of total hip replacement has resulted in not only more patients getting a hip replacement but a younger population getting replacement surgery.
The younger age group may have a higher level of functional goals as compared to the elderly population. Regardless of age, a thorough post operative exercise protocol is necessary to prevent range of motion and strength related issues after total hip replacement.
A progressive rehabilitation is recommended after the surgery as patients may be wary of any activity after the surgery. During the initial postoperative period, patients may complain of pain and swelling of the hip region secondary to the surgery.
Following resolution of the initial pain with medications, icing and rest a physical therapy protocol is initiated to increase flexibility, strengthen the muscles and improve balance and activities of daily living such as walking, stairs, etc.
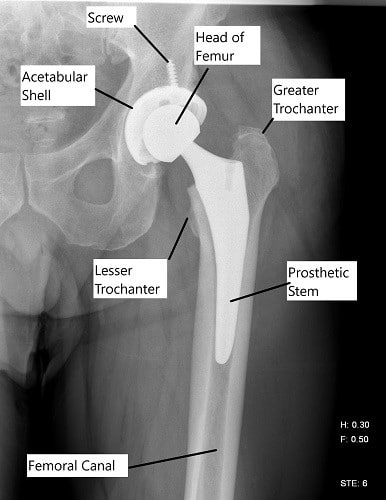
X-ray showing a total hip replacement.
Certain precautions need to be followed before resumption of the exercise program. The precautions may be different depending upon the type of approach used in the surgery and the stability of the surgery.
Certain common precautions after posterior approach include, avoiding bending at the hip past 80 degrees (such as sitting on a very low chair), avoiding inward movement of the toes (such as while tying shoe laces) and avoiding to cross the affected side over the normal side (as while sleeping on the normal side).
Precautions advised after an anterior approach include avoiding excessive backward bending at the hip and avoiding excessive outward movement of the toes. These movements may lead to dislocation of the artificial joints especially in the immediate postoperative period.
Exercise after hip replacement not only reduces the incidence of dreaded blood clots but improves circulation of the legs, helps strengthen the muscles and increases flexibility. The increase in blood supply following surgery helps in early healing of the incision and tissues.
While initiating exercise it is important to repeat them regularly 3-4 times a week and to do progressive reputations and sets. During the early post operative period, majority of the exercises may be performed even while lying down.
- Tighten your buttocks and hold them in contraction for a count of 5-6 seconds. Release and repeat the contractions at least 10-15 times a day.
- Bend your knees while maintaining the feet on the bed as the heel progressively touches your buttock. Try to hold it for a few seconds and then release and repeat.
- While lying down, try to push your knee against the bed, you will feel your thigh muscles contracting as you do so. Keep the thigh muscles contracted for a few seconds. Release and repeat multiple times during the day
- Quadriceps muscles may also be strengthened with straight leg raises. Try to tighten the thigh muscles and lift your leg a few inches off the bed. Hold the leg for a few seconds and then repeat.
- Try to move the leg away from the body to the side as far as you can and then bring the leg back. Repeat multiple times during the day.
- Ankle pumps consist of pressing the ankle down with your toes pointing. The exercise is recommended immediately after the surgery and advised to be repeated multiple times a day.

Intraoperative image showing a total hip replacement.
Standing exercises may be started after the patient is comfortable walking and has adequate balance. Standard exercises are advised to be done in presence of your therapist. Some of the standing exercises are :
- Stand with the support of the back of a chair and try to lift your one knee up until your waist level. Try to hold your knee at the level and then slowly bring it down.
- Quadriceps exercises may also be performed in a sitting position in a chair. Try to straighten your leg while sitting in a chair. Hold your straight leg while contacting the thigh muscles and then slowly bring the leg back.
- Similarly, standing with support of a chair, try to lift your leg to the side as far as possible and then bring it slowly back.
- Hip extension exercise consists of trying to bend your hip back and then bring it to a neutral position. However hip extension exercises may not be recommended when the hip replacement is done via an anterior approach.
- Heel rises is done with help of your therapist and consists of holding the hands of your therapist and trying to lift your heels off the ground. Hold the lifted heels in position for a few seconds and then bring them back slowly.
Soreness as a result of exercise is normal. However, any kind of pain is abnormal and it is advised to discontinue exercise for at least 2 days and then start gradually again.
Besides exercises, special emphasis is placed on walking and gait training. The therapist works to assess your walking pattern and to help you learn proper walking techniques. The patients are advised to walk the first day following surgery.
An assistive device in the form of a walker may be used. The patients are advised to always keep the walker in front of them at a comfortable distance to prevent inadvertent falls. The patients are also advised to first touch their heel and then rest of the foot while walking.
Walking training is followed by training in balance and activities of daily living such as climbing up and down the stairs. After the initial postoperative exercise training and gait training, advance training may include elastic bands to increase resistance training.
Gradually progressive exercises after a total hip replacement has shown to improve function and decrease pain after the surgery. Participation in exercises lead to early resumption of the activities the patients enjoy. The exercise program is specially tailored according to the patients needs and the type of the surgery.
Do you have more questions?
What exercises can I perform immediately after hip replacement surgery, and how frequently should I do them?
Exercises such as ankle pumps and buttock contractions can be initiated soon after surgery. Your therapist will provide guidance on frequency and progression based on your individual needs.
Are there specific exercises I should avoid during the initial postoperative period?
Certain movements, such as excessive bending or twisting at the hip joint, may be restricted initially to prevent strain on the surgical site. Your therapist will outline any precautions you should follow.
How can I differentiate between normal soreness after exercise and abnormal pain that may indicate a problem?
Normal soreness may occur after exercise, but any sharp or persistent pain should be reported to your healthcare provider. They can help determine if the pain is within expected limits or requires further evaluation.
Are there any assistive devices or equipment that can aid in performing exercises safely during the recovery period?
Depending on your mobility and balance, your therapist may recommend using assistive devices such as a walker or cane to support you during exercises and activities. These tools can help prevent falls and promote stability.
What strategies can I use to stay motivated and consistent with my exercise program during the rehabilitation process?
Setting realistic goals, tracking progress, and engaging in activities you enjoy can help maintain motivation during rehabilitation. Working closely with your therapist and celebrating milestones can also provide encouragement.
When can I expect to transition from lying-down exercises to standing exercises, and what signs indicate readiness for this progression?
The timing of transitioning to standing exercises varies for each individual and depends on factors such as pain levels and surgical recovery. Your therapist will assess your readiness based on your progress and symptoms.
How can I incorporate exercise into my daily routine to ensure consistency and maximize benefits?
Integrating exercises into daily activities, such as performing leg lifts while seated or taking short walks throughout the day, can help maintain consistency and enhance rehabilitation outcomes.
Are there specific precautions I should take when performing exercises to ensure the longevity of my hip replacement?
Avoiding high-impact activities and adhering to movement restrictions recommended by your surgeon can help protect your hip replacement and minimize the risk of complications. Your therapist can provide personalized guidance.
Can I engage in activities such as swimming or cycling as part of my exercise regimen, and if so, when can I start?
Low-impact activities like swimming and cycling can be beneficial for rehabilitation, but the timing of initiation should be discussed with your healthcare provider. They can advise on when it’s safe to incorporate these activities based on your recovery progress.
What modifications, if any, should I make to my exercise routine as I progress through different stages of recovery?
As your strength and mobility improve, your therapist may introduce more challenging exercises or modify existing ones to continue advancing your rehabilitation. Regular reassessment ensures your program remains tailored to your evolving needs.
What should I do if I experience discomfort or difficulty performing certain exercises?
If you encounter discomfort or challenges with specific exercises, it’s essential to communicate this with your therapist. They can modify the exercises or provide alternative options to ensure your comfort and safety.
Can I perform exercises on my own at home, or should I always do them under the supervision of a therapist?
While supervised sessions with a therapist are beneficial initially, many exercises can be safely performed at home once you’re familiar with them. Your therapist will provide instructions on proper technique and precautions for home exercise.
Are there specific signs or symptoms I should watch for during exercise that may indicate a complication or problem with my hip replacement?
Signs such as increased pain, swelling, instability, or unusual sensations around the hip joint during exercise may warrant further evaluation. It’s essential to promptly report any concerning symptoms to your healthcare provider.
What role does flexibility training play in my rehabilitation, and how can I incorporate it into my exercise routine?
Flexibility exercises help improve joint mobility and reduce stiffness, which is crucial for optimal recovery after hip replacement surgery. Your therapist can recommend stretches and techniques to enhance flexibility safely.
How long should I continue with my exercise program after hip replacement surgery, and are there long-term benefits to maintaining an active lifestyle?
Exercise should be viewed as a lifelong commitment to maintaining joint health and function. Continuing with a tailored exercise program can help prevent muscle weakness, joint stiffness, and other issues associated with hip replacement in the long term.
Are there specific dietary or lifestyle factors that can support my recovery and enhance the effectiveness of my exercise program?
A balanced diet rich in nutrients, along with adequate hydration and sufficient rest, can complement your exercise regimen and promote overall healing and recovery. Your healthcare provider can provide personalized recommendations.
Can I participate in group exercise classes or sports activities after hip replacement surgery, and are there any limitations or precautions I should be aware of?
Engaging in group exercise classes or sports activities can be enjoyable and beneficial for physical and social well-being. However, it’s essential to choose activities that are low-impact and joint-friendly, and to follow any movement restrictions advised by your surgeon.
What should I do if I experience setbacks or plateaus in my rehabilitation progress despite consistent exercise?
Setbacks and plateaus are common during rehabilitation, but they can often be overcome with adjustments to your exercise program or additional support from your healthcare team. Open communication with your therapist allows for timely interventions and modifications as needed.
Are there specific strategies or techniques for managing pain or discomfort during exercise, especially in the early stages of recovery?
Utilizing pain management techniques such as icing, elevation, and medication as prescribed by your healthcare provider can help alleviate discomfort during exercise. Your therapist can also teach you positioning and movement strategies to minimize pain.
How can I ensure that I’m performing exercises correctly and effectively to achieve the best possible outcomes?
Regular communication with your therapist, adherence to prescribed guidelines, and careful attention to proper technique are essential for maximizing the benefits of exercise. Your therapist can provide feedback and guidance to ensure correct execution.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

