Case Study: Shoulder Arthroscopy: Rotator Cuff Repair
Acromioplasty and Subacromial Decompression
and Distal Clavicular Excision in a 65 year-old patient
An arthroscope, a tiny camera used in shoulder arthroscopy, is inserted into your shoulder joint by the surgeon. Your surgeon uses the images from the camera to guide tiny surgical tools as they are displayed on a television monitor.
One’s range of motion may also vary, along with symptoms including pain, swelling, numbness, tingling, weakness, changes in temperature or color. The most frequent causes of shoulder injuries include sports-related activities, work-related duties, home improvement projects, and falls. Minor aches and pains may frequently be relieved at home.
A 65 year-old patient was in our office with complaints regarding neck, left shoulder, upper and lower back pain. Patient did not have pain in these body parts before the current injury. For aggravating factors, patient reports standing and lifting.
For location, left. For quality, throbbing, sharp, and constant. For severity, she reports moderate. For the date of onset, she reports 11-1-21. For timing, acute. For context, she reported mva. For alleviating factors, ice, rest, and otc medication.
For associated symptoms, no weakness, no numbness, no tingling, no swelling, no redness, no warmth, no ecchymosis, no catching/locking, no popping/clicking, no buckling, no grinding, no instability, no radiation, no drainage, no fever, no chills, no weight loss, no change in bowel/bladder habits, and no tenderness.
The patient presented results for MRI in cervical spine and showed posteroventral disc herniations at C4-C5 and C6-C7, which indent the ventral thecal sac and ventral cord surface. Annular bulge/vertebral spurring at C5-C6, associated with bilateral uncovertebral spurring, slightly larger on the right.
Findings result in, mass effect on the thecal sac and spinal cord, bilateral foraminal encroachment, and slightly worse on the right. Mild cervical spinal stenosis. Facet joint arthropathy in the upper cervical region, more marked on the left.
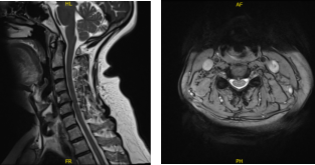
MRI Cervical Spine non-contrast
MRI results for her shoulder were also presented and showed full-thickness tear of the supraspinatus tendon spanning 1.4 cm in AP dimension. Tendinosis and partial-thickness articular sided tearing in the infraspinatus tendon spanning 0.8 cm in AP dimension.
Partial tear of the superior subscapularis tendon. Large fatty mass within and deep to the tree’s minor muscle measuring 6.8 x 3.7 x 4.3 cm without patient’s or solid components.
The mass abuts the posterior margin of the glenoid and portions of the posterior aspect of the humeral head and neck. Moderate glenohumeral joint effusion. Undersurface spurring of the acromion with increased risk of subacromial impingement.
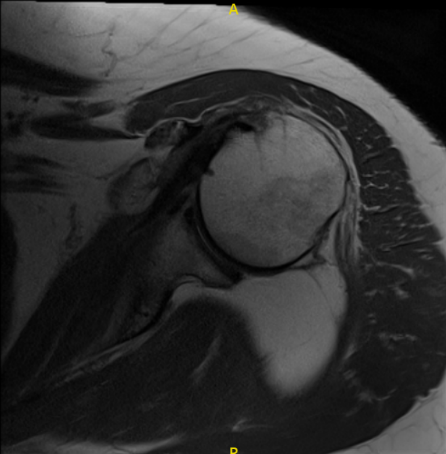
MRI Left Shoulder non-contrast
The anesthesia team administered a supraclavicular block in the pre-op area. A well-padded operating table was used when the patient was brought into the operating room. After being given sedation, she was positioned with her right shoulder up and her left shoulder lateral.
Well-padded bony prominences on all sides. The bean bag kept her firmly in place. A roll of the axilla was inserted. The right shoulder was prepared as normal and wrapped aseptically. A timeout was ordered. An antibiotic was administered before the surgery.
Because it was difficult to reach the glenohumeral joint through the soft spot, an arthroscope was introduced into the subacromial region. The MRI revealed no disease in the glenohumeral joint. The subacromial area was examined and found to have subacromial bursitis, which was debrided with a shaver.
The supraspinatus has partial thickness ripping around its insertion into the larger tuberosity. Anterior acromial spurring with impingement was seen. A coblation wand was used to loosen the coracoacromial ligament as well as to clean and prepare the acromion for acromioplasty.
The acromial spur was removed with a bur, and the acromioplasty was performed. It was decided to reconstruct the supraspinatus tendon with a Regeneten medical rotation implant. It was introduced via the lateral portal.
To place the tacks, an auxiliary superior gateway was created. It was attached to the rotator cuff tendon with PLLA tacks placed in the tendon region. Two bony tacks were used to secure it over the bone. The final photographs were shot and preserved.
The shoulder had been watered and drained completely. Layers of 2-0 Vicryl and 3-0 nylon were used to close the gap. Adaptic, 4 x 4’s, ABD, and tape were used for dressing. In stable condition, the patient was placed in a shoulder sling and transported to recovery.
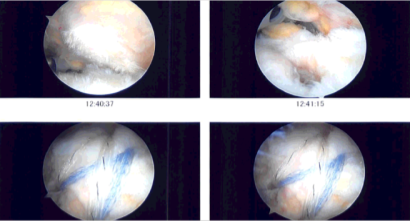
Intraoperative Arthroscopy Images
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the shoulder. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her shoulder.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

