Case Study: Shoulder Arthroscopy: Rotator Cuff Repair
in a 73 year-old man
A minimally invasive procedure called shoulder arthroscopy is performed to identify and treat shoulder issues. For shoulder impingement or rotator cuff injuries, you might undergo an arthroscopy. Smaller incisions are needed for minimally invasive procedures than for conventional surgery.
The size of each cut is comparable to a keyhole. The purpose of rotator cuff repair surgery is to reduce pain that is resistant to conventional therapies and to help the shoulder regain its flexibility and function.
The patient, a 73 year-old man, came to my clinic complaining of left shoulder ache following a fall. Before that, he had been experiencing left shoulder ache. He was unable to lift his left shoulder since he had lost all function in it.
After performing an MRI, it was discovered that the left shoulder’s supraspinatus and infraspinatus were completely torn. Biceps tendon absence was also visible.
We spoke about our alternatives for treatment and decided on surgical treatment. Infection, hemorrhage, damage to nearby nerves and blood vessels, failure to heal, need for a second operation, need for replacement in the future, and potential need for biceps tenodesis were just a few of the risks and benefits we reviewed.
We talked about systemic issues such as blood clots, cardiac, pulmonary, and neurological issues like death. The client was aware and gave informed consent.
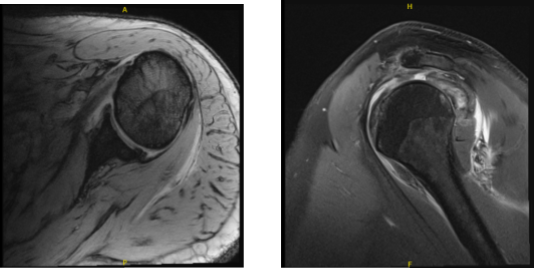
MRI-3T Left shoulder non-contrast
The patient was brought into the operation room and placed on a well-padded operating table. Anesthesia was administered. A timeout was issued. Clindamycin 900 mg was given as preoperative antibiotics. The patient was given a supraclavicular block prior to surgery. T
he patient was placed on his right side, with his left shoulder raised. As usual, the left shoulder was prepared and draped aseptically. A timeout was issued. The arthroscope was introduced into the glenohumeral joint through a posterior entrance site. A significant rotator cuff injury was visible.
The subscapularis was partially torn, which was debrided. The glenoid labrum had partial degenerative tears that were debrided. The spinal needle and shaver were utilized to create the entry portal and the dorsal medial portal for this debridement.
The scope was then advanced to the subacromial space, where subacromial decompression was performed using a shaver. A significant cuff rip was visible and prepped. A burr was used to prepare the footprint.
Two triple plate corkscrews were put on the anterior and posterior footprints at predetermined locations. Sutures were threaded through the rotator cuff tendon in a sequential fashion.
Before beginning the rotator cuff repair, an Allen Mason type of stay suture was used to approximate the supra and infraspinatus tendons. Sutures were passed successively and fastened together. The repair was deemed sufficient. The sutures had been punched.
Acromioplasty was performed with the Coblation band, followed by burr. AC arthritis was seen. The distal clavicle excision was performed with a Coblation wand, followed by a burr. A centimeter of the distal clavicle was removed. The final photographs were shot and preserved.
The shoulder was thoroughly cleaned, irrigated, and draped. The procedure for biceps tenodesis was postponed due to the lack of the biceps and the possibility of tendon fibrosis into the margins of the elbow.
This was planned and communicated with the patient prior to surgery. The wound was closed with #4-0 nylon, and the dressing was applied using Xeroform.
After one week the patient is seen by the doctor for his post operative consultation, no x-rays are needed. His pain is well controlled, he denies fever or chills and he is using the shoulder immobilizer.
We chose to proceed with official physical therapy as well as a home exercise regimen for shoulder rehabilitation after examining treatment choices. During the visit, we removed the stitches. We will continue to use ice and elevate the shoulder to reduce swelling and pain.
We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications. We also covered the risks and benefits of taking these medications, as well as the most prevalent side effects. The patient will return in three weeks to assess their progress.
After one month the patient went to the office for his post operative consultation, no x-rays were needed. Just like before, his pain is well controlled, he doesn’t have any symptoms of fever and chills and he is still using the shoulder immobilizer.
We decided to use cautious management for the time being. PT will start. To lessen discomfort and swelling, we will still utilize ice and elevation, and we will keep taking over-the-counter anti-inflammatory medications. His follow-up 4 weeks later.
The patient returns to the office two months later for his post-operative consultation; no x-rays are required. His discomfort is effectively managed, and he has no temperature or chills. He is still wearing the shoulder immobilizer.
He is presently working with PT and making good progress. The patient’s progress and development have been undeniable with continued physical treatment and regular attendance at his follow-up checkups.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

