Case Study: Rotator Cuff Repair, Debridement, Subacromial
Decompression and Acromioplasty of the left shoulder
in a 56 year-old male patient
The patient is in our office self-referred to me with complaints of left shoulder and left knee pain for almost 7 months. The patient remembers the injury in a motor vehicle accident back then. The pain is severe in intensity. The patient describes the pain as sharp and stabbing.
The pain is constant and does disturb sleep. The pain is not associated with swelling, bruising, numbness, tingling, radiating pain, weakness, bowel or bladder abnormality, gait problem, or limping, giving way, hand function difficulty. The problem has been getting worse since it started.
Walking, lifting, exercise, kneeling, make the symptoms worse. Medication makes the symptoms better. The patient has undergone surgery on his left shoulder.
He presented his MRI to me, and we reviewed it. Impression as follows: Status post rotator cuff repair with marked metal artifact slightly limited examination. Suggestion of at least partial tearing of the supraspinatus tendon.
Consider CT arthrogram or ultrasound for further evaluation. High-grade partial tearing of the infraspinatus tendon with possible full-thickness component. Suggestion of biceps tenodesis.

MRI of the left shoulder
His examination was suggestive of a rotator cuff tear of the left shoulder. We discussed treatment options and opted for surgical management. The patient has undergone a rotator cuff repair of the left shoulder about six years back.
His functions were fully recovered after that surgery until this accident happened.
We discussed risks, benefits, complications of surgical treatment Including infection, bleeding, nonhealing, need for repeat surgery, need for shoulder arthroplasty in future, injury to adjacent nerves and vessels, rehabilitation, systemic complications including blood clot, cardiac, neurological, pulmonary complications including death.
The patient understood and signed an informed consent.
The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced. A supraclavicular block was given preoperatively. The patient was turned into the right lateral position with the left shoulder up.
He was held in excellent position in the beanbag. Axillary roll was used to pad the axilla. All the bony prominences were well padded. The left upper extremity was prepped and draped aseptically in the usual fashion. Preoperative antibiotics
Lateral entry portal was made. The scope was entered. Examination of the glenohumeral joint showed extensive synovitis, degenerative arthritis of the glenohumeral joint more on the humeral head, absence of biceps and the rotator cuff tear in the region of supraspinatus and in infraspinatus.
An anterior entry portal was made and shaver was introduced and debridement of the synovitis was performed. Chondroplasty of the humeral head as well as the glenoid was also performed. The scope was entered from the anterior portal and findings were re-confirmed and debridement was completed.
The scope was entered in the subacromial space. A limited examination tear was found in the supra and Infraspinatus region. Debridement was done and bursa was removed. There was acromial spur anteriorly. The spur was removed by the use of a burr.
Acromioplasty was performed. A decision was made to repair the rotator cuff. An accessory left portal was made. The footprint for the rotator cuff was debrided using a burr exposing the subcortical bone. Then, a 4.5 mm with four tails was used and Inserted Into the humeral head following and tapped.
All the four tails were passed through the rotator cuff sequentially from anterior to posterior edge. The tails were tied over each onto itself using a sliding knot. The rotator cuff was well opposed. Final pictures were taken and the shoulder was irrigated.
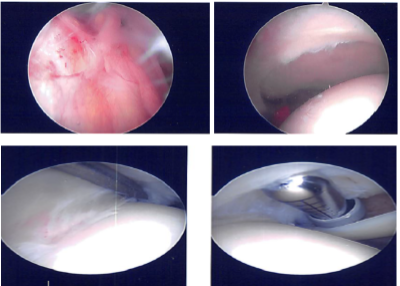
Intraoperative Arthroscopy Images
After a week post-operative, the patient consulted again in our office. He is doing fine and his pain has improved. He is using a shoulder immobilizer. Examination of the left shoulder reveals that the incisions are healing well, without evidence of drainage, erythema or warmth.
Range of motion and strength are progressing appropriately at this stage of rehabilitation. Strength remains 5/5 distally. There is no tenderness at the elbow and wrist. Sensation is intact to light touch distally and there is a brisk capillary refill.
We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

