Case Study: Patellar Tendon Repair Performed
to 61-year-old male patient
Tendons play an important part in the human skeletal system. It connects our muscles to our bones, and our bones allow our bodies to move easily. Tendon damage can be caused by overuse, injury, aging, and medical disorders such as arthritis.
A tendon rupture is a serious issue that can cause excruciating pain and permanent disability if left untreated. In this article, tendon repair and recovery treatment were discussed to an old male patient due to his previous injury.
Patient is a 61-year-old male presented today in the office with complaints of right leg and knee pain. The patient was at Penn station walking down stairs when he fell. The patient was taken to NYU emergency room. X-rays were taken and he was splinted. The pain is associated with swelling, bruising, tingling, numbness, radiating pain, weakness, gait.
The problem has been getting worse since it started. Walking, standing, lifting, exercise, twisting, lying in bed, bending, squatting, kneeling, stairs, sitting make the symptoms worse. Rest, ice, and lying down makes the symptoms better. The patient is a diabetic – on insulin, well controlled.
Xray and MRI results were presented and shown and no significant degenerative changes in the Xray. Meanwhile, MRI showed significant result of full-thickness rupture of the distal quadriceps tendon occurring 1.8 cm proximal to the patellar insertion site and resulting in a tear gap measuring up to 1.5 cm. There is accompanying patella Baja and soft tissue edema tracking into the vastus musculature and small to moderate-sized joint effusion.

Right Knee X-ray AP Lateral and Oblique 3 views
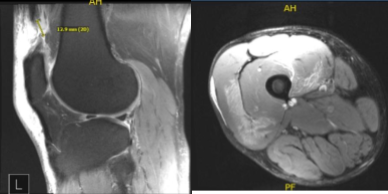
MRI-3T Right Knee Non-contrast
Upon examination of the right knee, the patient is tender to palpation along the distal aspect of the quadriceps tendon, and has an effusion. The patient has a palpable gap at the proximal aspect of the patella.
The patient cannot tolerate McMurray’s maneuvers or stability testing due to discomfort and swelling. They lack full range of motion. They cannot perform a straight leg raise and have weakness with extension. They are neurovascularly intact distally. There is no erythema, warmth or skin lesions present.
For quadriceps rupture right knee. We discussed treatment options including surgical and nonsurgical and their risks, benefits, and complications. The patient opted for surgical management.
We discussed regarding infection, nonhealing, failure, bleeding, need for transfusion, chronic knee pain, knee stiffness, arthrofibrosis, complex regional pain syndrome, need for rehabilitation, need for ambulation with crutches with locked knee in extension, knee arthritis, need for repeat surgery, need for knee replacement in the future amongst others.
We also discussed anesthesia complications including stroke, paralysis, cardiac, pulmonary complications including death. The patient agreed and signed an informed consent.
The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced and he was intubated. The right lower extremity was prepped and draped in a usual aseptic fashion after a tourniquet was applied over the upper thigh. Esmarch was used to exsanguinate the extremity.
A midline vertical incision was given centering over the superior pole of the patella to expose the distal quadriceps as well as the distal pole of patella. A complete tear of the quadriceps tendon was found.
The joint was exposed. Serosanguineous fluid was drained and the knee joint was washed thoroughly. The debridement of loose muscle and periosteal tissue was done.
The superior pole of patella was exposed and the pole was denuded and decorticated to prepare a bed for insertion of quadriceps. Three trans osseous tunnels were made from the superior pole to the inferior pole and suture passer was used to pass back sutures through the three tunnels.
Now, the quadriceps tendon was prepped and two #5 Fiber Wire were used to pass Krakow stitch on either side, 5 locking knots each limb or either suture. The sutures were passed into the patella through 3 trans osseous tunnels. The two central limbs were identified on either side and passed off to the side of their respective sutures.
The knee was put in full extension and the sutures were knotted on the inferior pole of the patella. The medial and lateral extensor retinaculum was repaired using 0 Vicryl
. The wound was again washed and closure of the wound was performed in layers using Vicryl #0 and Vicryl #2-0 followed by Monocryl #3-0 pull-out sutures. Steri-Strips were applied and dressing was done. Tourniquet was released. The patient was extubated and moved to the postoperative recovery unit in a stable condition.
After a week, the patient was presented for post operative check up. The patient is currently doing well. The patient continues to have mild pain. Symptoms are generally improving and there is no fever, chills or night sweats.
There is full compliance with all follow up instructions. On physical examination, there is mild swelling of the right limb compared to the left with no signs of infection or erythema.
The incision is clean and dry. There is no calf tenderness. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

