Case Study: ORIF: Displaced Lateral Malleolus Fracture
of the left ankle in a 78 year-old male
When the bone fragments are not out of place, a lateral malleolus fracture is characterized as nondisplaced. Surgery is usually required when bones are broken (fractured) and are out of place, unstable, or may become out of place.
This procedure is known as an open reduction and internal fixation (ORIF). The area of the fracture is opened up so the surgeon may see it during open reduction. Internal fixation refers to the use of screws, pins, or fixation devices to hold the bone parts in place.
A lateral malleolus fracture is a form of ankle fracture caused by the fibula breaking right above the ankle joint. The most common type of ankle fracture occurs when the foot rolls or twists.
A 78 year-old male patient visits the office with X-rays presented and complaints about the pain of his left foot and ankle after slipping on ice three days ago. The patient states that the pain has associated symptoms like swelling, instability, and tender to touch.
The X-rays were reviewed and discussed and he was diagnosed with Closed fracture of lateral malleolus – Displaced fracture of lateral malleolus of left fibula, initial encounter for closed fracture.
Upon the examination, we discussed the treatment options for the patient’s diagnosis, which included: non-surgical and surgical options. We discussed risks and benefits including infection, bleeding, nonhealing, need for repeat surgery, rehabilitation, injury to adjacent nerves and vessels. We also discussed systemic complications including blood clots, cardiac, pulmonary, neurological complications including death.
The patient understood and expressed a desire to proceed with surgery and signed the informed consent.
The patient was taken to the operating room where general anesthesia was induced. Preoperative antibiotic was already given. Hip bump was put under the left pelvis. Tourniquet was applied on the left side. The left lower extremity was prepped and draped aseptically in the usual fashion. A time-out was called.
A lateral malleolar incision, hockey-stick shape was given. Fascia was cut in the line of the incision. Fracture site was reached and cleaned. Curette was used to clean the fracture. The fracture was irrigated and washed.
The fracture was reduced using lobster clasp and an interfragmentary screw of 3.5 mm was inserted between the two compressions of the fracture. After the compression of the fracture, lateral malleolar plate was applied over the distal fibula and the plate was held with olive wires.
Pictures were taken and found to be satisfactory. The fixation of the plate was done to the distal fibula using a combination of locking and nonlocking screws. A total of seven screws to the plate and one interfragmentary screw was used. Final pictures were taken and saved.
The wound was thoroughly washed and closed in layers using #0 Vicryl, # 3-0 Vicryl, and # 4-0 Monocryl. Dressing was done using Xeroform and 4 x 4. Posterior splint was applied using Webril, fiber splint and Ace wrap. The patient was extubated and moved to Recovery in a stable condition.
After two weeks from the surgery the patient was seen in the office for his post operative visits, the doctor reviewed and discussed the X-rays. Surgical plate and screws transfix the distal left fibula with near-anatomic alignment. Hardware appears intact and the distal tibia is also intact.
Visualized aspects of the left talus, calcaneus and tarsal bones demonstrate intact cortical margins with no evidence of an acute fracture. There are no significant degenerative changes, the Ankle mortise is well maintained.
There’s mild soft tissue swelling. An overlying splint is noted and no calcaneal plantar spur. Which means that the Surgically treated fracture of the distal left fibula with near-anatomic alignment.
We discussed treatment options including PT, MRI, Injection, and the surgery. However, we agreed to go with conservative management for now, continuing with post splint, Ice and Elevation to ease the swelling and inflammation and using OTC anti-inflammatory meds to relieve pains. The patient follows up the checkup after 2 weeks with a walker boot and x rays.

Left ankle x-ray complete
After a month the patient was seen in the office for post operative consultation with an X-ray of his left ankle and he is also complaining of left knee pain which has worsened recently. The doctor reviewed the X-ray, he saw the sunrise patella and standing AP, lateral.
The distal femur, patella, proximal tibia and proximal fibula demonstrate intact cortical margins with no acute fracture. The medial, lateral and patellofemoral joint spaces are well-maintained however, there is mild medial, lateral and patellofemoral osteophyte formation.
There is no radiographic evidence of a joint effusion and no radiographic evidence of soft tissue swelling. It has no fractures but there are mild osteoarthritic degenerative changes.
We agreed to continue with conservative management for now, using Cam walker boot, PWB, Ice, Elevation and OTC anti-inflammatory meds. The patient will be back after 4 weeks for his follow up checkup with X-rays.
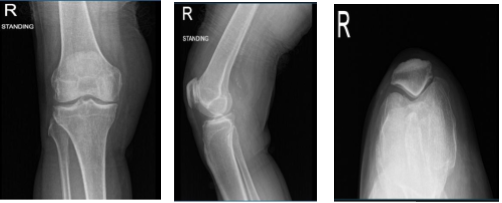
Right knee x-ray complete with patella
Another 2 weeks has passed, the patient seen in the office for his operative consultation. His therapist called informing that he is having swelling of the ankle which was concerning. The doctor reviewed the x-ray of the left ankle.
He has B/L hammer toes and is under care of a podiatrist and had recent swelling of the right second toe for which he has been prescribed antibiotics. Other months have passed and the patient has been improving. His swelling has decreased,
He occasionally walks FWB with boots and has minimal discomfort. He can now drive. The doctor reviewed the x-ray of the left ankle. He has B/L hammer toes and is under the care of a podiatrist. He still had swelling of the right second toe for which he may need surgery.
However, we agreed to continue with conservative management for now. Cam walker boot to continue, Crutches to be weaned off, the PT to continue, WBAT, Ice, Elevation and OTC anti-inflammatory meds.
Follow up checkup every 4 weeks with x-rays. With the continued follow up checkup the patient showed progress from time to time he visits the office. He gets well after the surgery and with the help of continuing physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

