Case Study: Knee Arthroscopy: Tear of Medial Meniscus
with Chondroplasty in a 44 year-old male
In chondroplasty or debridement, the articular cartilage is surgically shaped. To stabilize and treat chondral lesions, a procedure known as chondroplasty involves removing unstable cartilage flaps and smoothing out degenerating cartilage.
Total knee replacement is regarded as a relatively routine procedure, with 85% of patients reporting satisfaction, 10% not seeing a significant improvement, and 5% reporting worsening of symptoms.
The patient 43 year-old male presents with right knee pain since the car accident. He has tried PT, chiro, NSAIDs with no relief. He is back to work as conductor at LIRR. Pain was localized to the medial tibiofemoral joint line. The patient was treated conservatively for pain, but had failed.
We did an MRI, which showed a tear of the medial meniscus of the right knee. We discussed treatment options and opted for surgical management.
We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, need for repeat surgery, additional pain, need for knee reoperation, arthritis, need for knee replacement in the future, systemic complications like deep vein thrombosis, cardiac, pulmonary, and neurological complications including death. The patient understood and signed an informed consent.
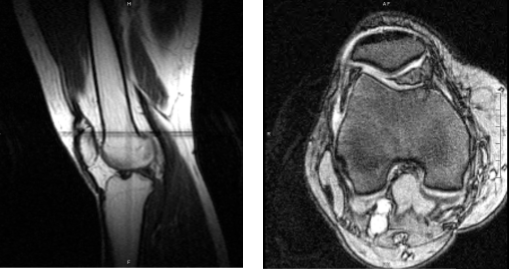
Magnetic resonance imaging of the right knee
In the operating room, general anesthesia was produced on the patient. The right lower extremity was prepared as normal and draped aseptically. A tourniquet was put around the low thigh. During the procedure, the tourniquet was worn for about 30 minutes at a pressure of 325 mmHg.
A timeout was ordered. Using a scalpel, the incision was made after preoperative antibiotics were already administered. The arthrometer was implanted. A spinal needle was used to create a medial entrance hole. The glenohumeral cartilage appeared to be intact upon examination.
Upon closer inspection, it was discovered that the medial meniscus had torn along its inferior and lateral margins, from the posterior body to the posterior horn, of the medial tibiofemoral compartment.
The meniscus and rongeurs were debrided with a razor and biters. The intercondylar notch examination revealed an undamaged ACL. When the lateral tibiofemoral compartment was examined, the meniscus and cartilage were both in good condition.
The medial portal was used to insert the arthroscope, and the entry portal was used for further debridement using the shaver. Final images were captured and stored. It was irrigated and drained completely. Using # 3-0 nylon, layers of closure were completed.
40 mg of Depo-Medrol was injected together with 30 cc of 0.5% Marcaine. Xeroform, 4 x 8, ABD, Webril, and Ace wrap were used for dressing. The patient was transported to recovery in a stable state after being extubated.
After one week the patient was seen in the office for his post-operative visits, he is recovering well. He denies fever and chills but he uses crutches. After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during the visit. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications. The patient will be back in three weeks’ time to evaluate their progress.
After one month the patient went back for his post-operative consultation. He is recovering well; he does not have fever or chills. He is able to walk unaided. He is now working with his physical therapy though he had an episode of swelling in between which has recovered.
With continued regular checkups, attending physical therapy and doing home exercises for the knee, the patient gets well and recovered.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

