Case Study: Knee Arthroscopy: Medial Meniscectomy
with Patellofemoral Chondroplasty in a 59 year-old female
To stabilize and treat chondral lesions, a procedure known as chondroplasty involves removing unstable cartilage flaps and smoothing out degenerating cartilage. Trimming shaky flaps from a torn meniscus creates a stable remaining meniscus after partial meniscectomy.
A portion of a tendon taken from your leg is used to replace a ruptured lateral patellofemoral ligament during the treatment. The primary goal of the LPFL reconstruction is to tighten and stabilize the knee joint.
The patient, a 59-year-old female, complained of pain on the inside and in front of her knee when she came to visit the doctor in the office. She tried physical therapy and anti-inflammatory drugs, but they were ineffective. We had an MRI, and it revealed patellofemoral arthritis and a complicated medial meniscus rupture.
We spoke about our alternatives for treatment and decided on surgical treatment. Among other dangers and benefits, we talked about infection, bleeding, damage to nearby nerves and blood vessels, repeated tears and the need for more surgery, recovery, the onset of arthritis, and the potential need for knee replacement in the future.
We also covered systemic problems, such as blood clots, cardiac, pulmonary, and neurologic issues. The patient gave informed consent and signed it.
In the operating room, general anesthesia was produced on the patient. She was set down on an operating room table that was well-padded. After a low-thigh tourniquet and Esmarch administration, the left lower extremity was prepared and draped aseptically in the normal manner. Antibiotics for surgery have already been administered. A timeout was ordered.
A lateral parapatellar incision was used to create an entry portal, through which an arthroscope was introduced. The patella and trochlea both had grade 1 to grade 2 osteoarthritic alterations upon examination of the patellofemoral compartment.
The posterior horn of the medial meniscus was torn, as evidenced by a medial tibiofemoral compartment examination. Spinal needle and blade were used to create a medial entrance hole. A shaver was used, together with biters and shaver, to clean the damaged meniscus.
Along the body of the posterior horn of the medial meniscus, a balanced margin was attained. Intact was the root. The medial tibiofemoral compartment’s cartilage was undamaged.
The intercondylar notch examination revealed an undamaged ACL. Meniscus and cartilage that were examined in the lateral tibiofemoral compartment were in good condition. Once more, a shaver was used to tease grade 1 to grade 2 osteoarthritic alterations in the patellofemoral compartment. Final images were captured and stored.
The findings were confirmed after the arthroscope was placed through the medial portal. It was irrigated and drained completely on the knee. Nylon # 3-0 was used for the closure.
The knee was then injected with 20 cc of 0.5% Marcaine and 40 mg of Depo-Medrol. ABD, Webril, Ace wrap, and 4 x 4 were used for dressing. The patient was transported to recovery in a stable state after being extubated.
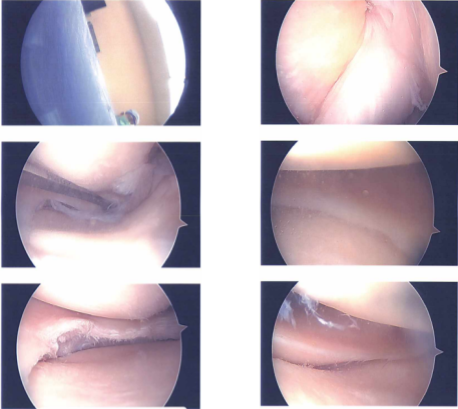
Intraoperative Images
After one-week, the patient was seen in the office for a post operative appointment, no x-rays needed. She denies fever or chills and her pain is well controlled. We discussed treatment options including PT, MRI, Injection, surgery and we agreed to go with conservative management for now.
After one month, the patient came in the office for her follow up checkup, it showed that the patient’s left knee is doing very well. She also has pain in right knee and she would plan the surgery in fall. We talked about many therapy possibilities, such as PT, MRI, injection, and surgery.
We decided to use cautious management for the time being. Ice/heat, elevation, over-the-counter anti-inflammatory drugs, cortisone injection under USG guidance, and physical therapy will all be initiated as discussed. She’ll be back in six weeks. If she doesn’t get relief from her right shoulder pain, consider arthroscopic debridement of the shoulder.
Three months later, the patient was seen in the office with worsening pain in right shoulder. She had a USG guided injection in 2016 which helped her. She got a cortisone inj in right shoulder (subacromial space) on 3/31/22 with no relief.
She had 3 injections under US guidance with the other physician, which did not help. MRI of the shoulder showed OA changes in the GH joint. Her shoulder is not getting better and she plans to get surgery done on it.
She is also status post arthroscopic surgery left knee medial meniscectomy, patellofemoral chondroplasty, injection of 20cc of 5% Marcaine mixed with 40mg of Depo Medrol performed on 4/6/22 at St. Catherine’s Hospital. She is doing well with her left knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

