Case Study: Transforaminal Lumbar Interbody Fusion
(TLIF) of Right L4-S1 in a 55-year-old Female
A 55-year-old female presented to our office with complaints of worsening lower back pain with radiation to the right buttock and posterior thigh. She first noticed the pain a year ago when she was involved in a motor vehicle accident. The pain subsequently worsened limiting her daily activities.
The pain is described as a sharp pain shooting down her right leg. The pain is especially worse on activities such as bending, sitting, getting up from a chair, walking, and climbing stairs. The intensity of the pain is described as severe (9/10). The pain interferes with her sleep.
The pain is associated with numbness and tingling in the right lower extremity. She denies any weakness in the lower extremities or any bowel bladder abnormality. The patient is currently unemployed on disability. Her past surgical history is significant for lower spine surgery 10 years ago and a total hip replacement was done 4 years ago.
Her medical history is significant for hypertension, hyperlipidemia, and hypothyroidism. She is currently taking metoprolol, pravastatin, and thyroxine. She had previously tried physical therapy along with hot and cold therapy. She received epidural and selective nerve root injections a year ago.
The patient is a former smoker and consumes moderate alcohol occasionally. She denies any known medical allergies. On physical examination, the patient is calm, conscious, cooperative, and well oriented to time, place, and person. Lower spine examination reveals tenderness over the right paraspinal musculature.
The range of the lumbar spine was limited secondary to pain. There is no tenderness on palpating the spinous processes. The straight leg raise test is positive at 60 degrees on the right side. There are no signs of erythema, swelling, ecchymosis, or draining sinus tracts.
Examination of the bilateral hips revealed no signs of tenderness over the trochanters with a full range of motion of both hips. The power sensory examination of the bilateral lower extremities was unremarkable with 5/5 strength and normal bulk and tone except right EHL 4/5. The sensory dermatomes were intact bilaterally except dorsal right foot Ist webspace. The deep tendon reflexes were symmetrical bilaterally. The power sensory examination of the bilateral upper extremities was unremarkable.
X-ray of the lumbar spine was reviewed with the patient. The X-ray revealed severe degenerative changes at L5-S1 and 5 mm anterolisthesis at L4-5.


Preoperative X-ray LS spine in AP and Lateral Views.
MRI of the lumbar spine was done to evaluate the L5 nerve root compression location. CT scan of the lumbar spine to review the bony anatomy and allow surgical planning. The patient had previously undergone an LS-S1 microdiscectomy approximately 15 years ago.
MRI revealed slight straightening of the lumbar spine. Lower lumbar discogenic degenerative disease with central canal stenosis resulting in impingement of the descending L5 and S1 nerve roots, respectively at L4-L5 and L5-S1 levels. The exiting right L4 nerve root is also impinged upon at L4-L5 and the exiting right L5 nerve root is impinged upon at L5-S1.
Lower lumbar facet arthrosis most present at L4-L5 where there is severe left greater than right arthrosis and a moderate left facet joint effusion.
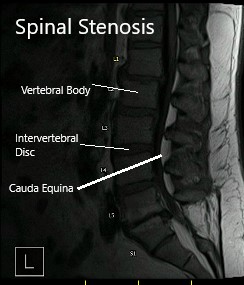
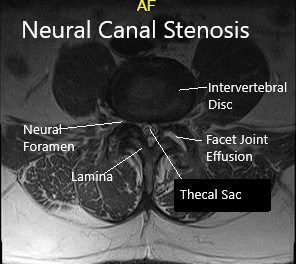
MRI showing sagittal and axial sections.
The patient had exhausted all conservative management options and was advised Minimal Invasive (MISS) Transforaminal Lumbar Interbody Fusion (TLIF) surgery. Risks, benefits, and alternatives were discussed thoroughly with her and her daughter. She agreed to go ahead with the surgery.
The patient was brought to the operating room and sedated under general endotracheal tube intubation. He was then placed in a prone position with adequate padding under all bony prominences.
His lower lumbar spine region was then prepped and draped in a usual sterile fashion and we then proceeded to use fluoroscopic imaging to identify the area for Wiltse approach for the minimal invasive transforaminal lateral interbody fusion.
Once we are satisfied with the positioning, we then chose a point approximately 3 cm lateral to the midline and approximately 4 cm in length. Once initial skin incision was made, we then used electrocautery to dissect down along the planes and identified the lumbar fascia. We then incised along the fascia and placed a stay suture within the fascia.
We then used blunt dissection to split the muscle fibers and palpated the edge of the transverse process. Once we are satisfied with the positioning on the fluoroscopic imaging, we then proceeded to use a Jamshidi needle onto the lateral tips of the facet joints except for the L4 region where it was placed along the corner of the transverse process and the facet in order to avoid injuring the L3-L4 facet joint.
All needles were placed under fluoroscopic imaging and once we were satisfied with the positioning, we then evaluated his nerve monitoring and found there to be no changes within any of the needle positions. We then proceeded to place a guidewire into the vertebral body and then removed the Jamshidi needle.
We then secured the guidewires onto the edge of the patient’s bed and turned our attention towards performing the decompression and interbody fusion procedures. We then used a microscope to began our decompression at the L4-L5 region.
We first identified the L4 lamina and performed a hemilaminectomy procedure. We were able to identify the dura as well as the exiting L4 nerve and we then identified the intervertebral disc space. There was a very large osteophyte complex along the L4-L5 region as well as the L5-S1 area.
We then continued our dissection using the Midas burr to also perform a hemilaminectomy of the L5-S1 region beginning with the L5 lamina and exiting up through the L5-S1 foramina. We were able to visualize the L5 nerve and completely decompress the nerve from any overlying tissue. We then identified the intervertebral disc space.
The disc space was significantly narrow with a notable amount of scarring around the dura to the disc. Once the decompression was complete and we were completely satisfied with the exposure, we then turned our attention towards the interbody fusions.
A size #15 blade was used to make an opening incision along the posterolateral annulus and we then proceeded to perform a microdiscectomy procedure. We used curettes from a Medtronic system and once we are satisfied with the discectomy, we then turned our attention towards placing an appropriately sized interbody implant.
Based on fluoroscopic imaging, we felt that a size #12 implants would be satisfactory and therefore we proceeded to obtain a crescent PEEK cage measuring 30 x 12 mm and packed it with demineralized bone matrix as well as BMP. We then proceeded to place the cage into position. The edge of the inferior L4 vertebral body was removed using an osteotome in order to allow for the entry of the implant.
Once we are satisfied with the positioning of the implant, we then evaluated its position on the both AP and lateral planes and proceeded to place bone graft posteriorly behind the implants within the intervertebral body. We then washed up the area with normal saline and reevaluated the nerve root and dura.
There were no signs of compression and we are really satisfied with the positioning and alignment of the interbody fusion implants and bone graft. We then turned our attention towards the L5-S1 region. Similarly, we used a size #15 blade to create an annulotomy and then proceeded to place several curettes in order to perform a microdiscectomy and prepare the intervertebral space for an implant.
We used the left side screws to distract the space open, but noted that there was very minimal opening. Similar to the L4-L5 region, we used an osteotome along the edge of the inferior L5 vertebral body in order to obtain an entry point. We then proceeded to place a size 30 x 9 mm crescent PEEK cage into position also using BMP and demineralized bone matrix into the implant.
We then evaluated the L5 exiting nerve root as well as the traversing S1 nerve root and the dura and found it to be completely decompressed. We were completely satisfied with the positioning and alignment of the implants and turned our attention towards the fixation of the rod and screws.
We first began with the left side and placed a size #60 mm length rod into position. We then secured it and ensured that there was an adequate amount of lumbar lordosis. We then also secured the right side rod with a similar length into position.
We then obtained final fluoroscopic images and were completely satisfied with our fixation and alignment. We then washed out the wounds with normal saline and vancomycin instilled into the wound. We proceeded to close the layers with a size #2 Vicryl sutures for the fascia layer followed by size #2-0 Vicryl suture for the subcutaneous skin and a running #4-0 Monocryl suture for the subcuticular layer.
Steri-Strips and dry dressings were placed onto the wound and the patient was then safely returned back to the recovery room. There were no intraoperative complications reported by the anesthetist. The nurses reported a correct instrument count.
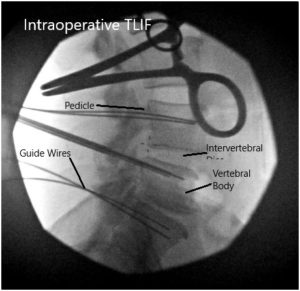

Intraoperative Fluoroscopic Images.
The patient will be allowed to weight bear as tolerated in the postoperative. We will ask him to refrain from nonsteroidal anti-inflammatories. The patient required only VTE prophylaxis while in the hospital. Paitent was discharged home after 4 days of hospital stay. He was followed as outpatient to an uneventful recovery. He was able to perform activities of daily living soon after the surgery and was back to baseline in about 10 weeks.
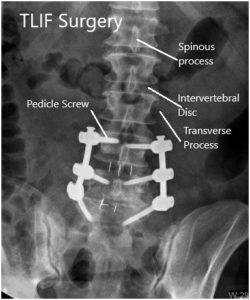
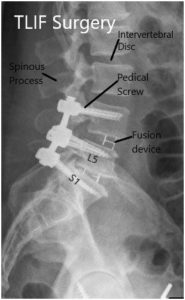
Postoperative X-ray in AP and Lateral views.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

