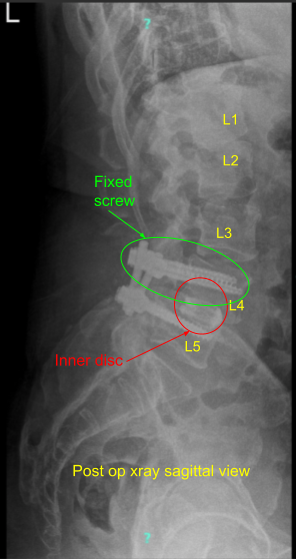
Case Study: Revision decompression of L4-L5
The patient was operated on L4-5 for grade 1 spondylolisthesis for symptoms of radiculopathy which were not relieved with conservative management. The patient did well after the surgery and had good pain relief till a couple of months after the surgery when they started having pain in both lower extremities which had been worsening.
They started having claudication symptoms. They were seen by us and new imaging had been done which showed collapse of the L4-L5 interdisc space along with loosening of setscrew of the left L4.
We discussed treatment options including surgical and nonsurgical treatment. The patient opted for surgical management but They wanted to delay it. They came back again because of worsening pain and were admitted to the Emergency Room (ER) of the St. Catherine’s Hospital because of the worsening pain and weakness in both lower extremities because of pain.

We did imaging which showed stenosis of the L4-5 along with possible infection because of fluid collection. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, CSF leak and need for repair, possibility for repeat surgery, inability to relieve the pain, systemic complications including blood clot, cardiac, pulmonary, and neurological complications including death. The patient understood and signed an informed consent plan to revision decompression of L4-L5.
The patient was taken to the operating room where general anesthesia was induced. Neuromonitoring was established. Foley catheter was passed. The patient was turned to a prone position on a four post Jackson table.
All the bony prominences were well padded. The surgical area was cordoned with use of 10 x 10 drapes and prep was done with the use 70% alcohol followed by DuraPrep. Draping of the back was done in the usual aseptic manner. Time-out was called.
The incision was created along the same previous incision. The incision was extended proximally. Deep dissection was done along the line of incision. The spinous process of L3 and L5 were exposed to find normal territory. The dissection was carried out deep and laterally on to the screws.
The set screw from left L4 was found to be dislodged into the soft tissue. It was removed. Further dissection was done on the transverse process of the L4 on the right side There was soft callus present. The decortication of L4 and L5 transverse processes and the pars was performed with intent to achieve fusion in the region.
A small BMP was opened in preparation for the fusion. Revision decompression of the L4-5 was performed with inferior laminectomy of the L3. The bone was used for local autograft. A thorough decompression of the L4 and L5 of the left and right was performed with the use of curettes followed by Kerrison punch. Full decompression could be achieved. A new set screw was put on to the left L4 and torqued in the usual fashion.
Final pictures were taken and saved. The wound was thoroughly irrigated. One-fourth of the small BMP strip was used and put on the right side followed by autograft and cancellous chips to achieve fusion. The wound was thoroughly irrigated and draped. Hemostasis was achieved with the use of Bovie,

Bipolar closure was performed with the use of #0 Vicryl. Vancomycin 1 g was sprinkled. Fascia was closed with the use of #0 Vicryl, subcutaneous tissue was closed with the use of #2-0 Vicryl, and skin was used with the use of #2-0 Monocryl.
Dressing was done with the use of Aquacel. The patient was turned supine on the bed and extubated.They were moving all four extremities and were extubated. The patient was moved to recovery in a stable condition.
Patient’s next office visit was one week status post L3-5 decompression and L4-5 PSF with improving neurologic involvement (urinary incontinence). Patient was followed in our office on regular intervals of 2 weeks, 6 weeks, 3 months and 6 months thereafter with gradual return of function. Physical therapy was also started. Patient did well postoperatively
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.

