Case Study: Management Of 58-Year-Old
Female With Burst Fracture Of T6 Vertebra
A 58-year-old female patient, who was involved with a fall where she slipped and landed on her back on some stairs. She was seen at another hospital where an incomplete workup was done and she was sent home. Unfortunately, her pain became worse and she was unable to carry out her activities of daily living despite aggressive medical management.
She presented to the emergency room at the Hospital in excruciating amounts of pain. An imaging workup revealed a burst fracture of the T6 vertebral body with more than 50% loss of height and acute angulation at that level, which worsened with flexion and extension.
The pain was described as sharp pain with a severe intensity (10/10). The pain was non-radiating and located in the upper mid-back. The pain was worse with movements. There was a paraspinal tenderness.
She had no power sensory deficit in the bilateral upper limbs and the lower limbs. There was no bowel or bladder dysfunction. The deep tendon reflexes were present and symmetrical bilaterally. Babinski reflex was indeterminate and Hoffman’s reflex was absent.
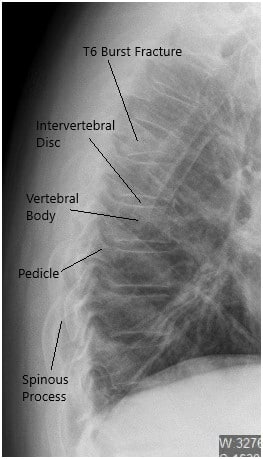
Preoperative X-ray of the Thoracolumbar Spine in Lateral View.
CT revealed moderate acute wedge compression fracture associated with the T6 vertebral body. The posterior cortex of the T6 vertebral body mildly impresses upon the anterior margin of the thoracic dural sac. Minimal hematoma is situated between the T6 vertebral body and the surrounding pleura.
There was a normal configuration of the remaining thoracic vertebral bodies. The thoracic disc spaces are not narrowed. Posterior disc bulges or herniations are not demonstrated. The narrowing is not associated with the thoracic neural foramina.
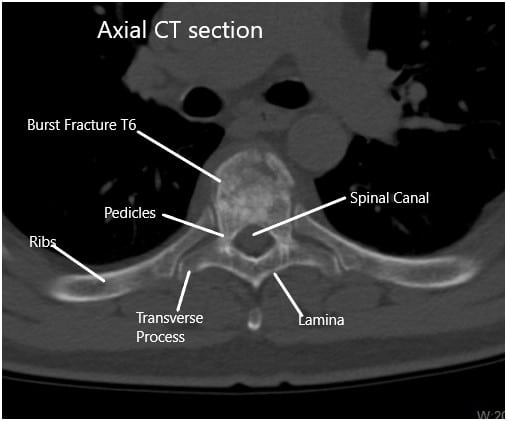
Preoperative CT Scan of the Thoracolumbar Spine in Axial Section at T6
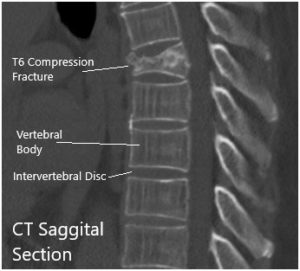
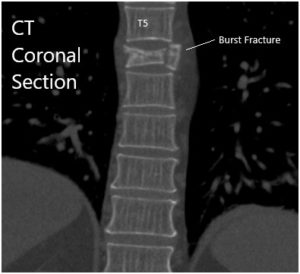
CT Sagittal and coronal Sections.
Given the acute fracture with biomechanical instability and unremitting back pain with a burst fracture compromising the spinal canal, we considered this a neurosurgical emergency and we offered the patient stabilization. She understood all the risks, benefits, and alternatives to surgery and she agreed to give informed consent for spine surgery.
PREOPERATIVE DIAGNOSIS: T6 burst fracture with acute kyphosis after a fall.
POSTOPERATIVE DIAGNOSIS: T6 burst fracture with acute kyphosis after a fall.
OPERATION:
- T6 kyphoplasty.
- T5 to T7 segmental instrumentation.
- T5 to T7 posterior arthrodesis and fusion with the use of morselized autograft and allograft.
- Use of intraoperative fluoroscopy.
- Use of intraoperative neuromonitoring.
- Bilateral transpedicular biopsies.
ANESTHESIA: General endotracheal anesthesia.
ESTIMATED BLOOD LOSS: 50 mL.
PROCEDURE IN DETAIL: The patient was identified in the preoperative holding area and then brought back to the operating room where he was induced under general anesthesia and intubated. A foley catheter was inserted and the patient was turned prone after neuromonitoring electrodes were attached.
He was secured onto an open bottom Jackson table and all of his pressure points were padded appropriately. The patient’s thoracic region was prepped and draped in the usual sterile fashion after using fluoroscopy to identify the level of operation. A time-out was called and preoperative antibiotics were dosed.

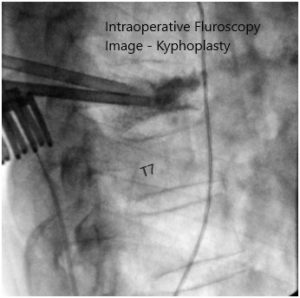
Intraoperative fluoroscopy images.
We marked a midline incision with an indelible marker and then used a #10 blade to incise the skin down to the level of the subcutaneous fat.
At this point, we used Bovie cautery to complete our dissection exposing the T5 through T7 lamina and we kept all the posterior elements intact. Using the NuVasive Maxcess retractor system, we held the muscle and skin edges apart.
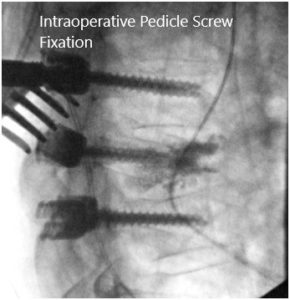
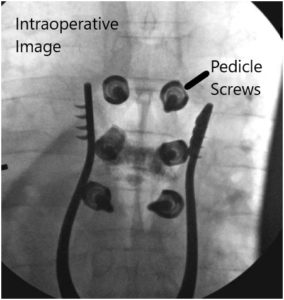
Intraoperative fluoroscopic images.
We employed fluoroscopy once again to check our level of operation and extended our incision slightly in the cephalad direction. At this point, we confirmed the level of the T6 vertebral body and started our open kyphoplasty.
First we inserted the Jamshidi needles under fluoroscopy through the pedicles to the vertebral body. We then inserted the cannulas for the kyphoplasty system bilaterally and obtained transpedicular biopsies, which were sent for histopathology.
At this point, we inserted the balloon on the patient’s right side and inflated it with contrast up to approximately 380 mmHg and this was checked constantly under both AP and lateral fluoroscopy simultaneously. We inflated the balloon to approximately 2 mL maintaining the pressure and to ensure that we remained within the confines of the vertebral body with the balloon inflation.
We did this then on the left side as well. The balloons were then deflated and removed and cement was introduced in a semi-liquid state, first on the right side, and then on the left side. Approximately 4 mL of cement was introduced from the right side and approximately 1.5 mL of cement was introduced from the left side.
There was an alarming amount of fracture at this level and the cement was maintained posterior to the anterior border of the vertebral body and anterior to the posterior border of the vertebral body. There was a small amount of extravasation of cement into the superior and inferior endplates.
At this point, given the location of the fracture and the severity, we then moved to finish our instrumented fusion from T5 to T7. The pedicles of T6 were cannulated by using the high-speed drill to create a starting point and then we used the pedicle gearshift under fluoroscopy to enter the pedicles.
Using anatomic trajectories, we then tapped these pedicles to start and inserted 4.5 x 30 mm pedicle screws on both sides. We confirmed our trajectories using fluoroscopy and triggered EMG. We did the same thing for both the T5 and T7 pedicles probing them using Lenke gearshifts and under fluoroscopy after creating our pilot hole with normal anatomical starting points with the high-speed drill. We inserted 5.5 x 40 mm screws under direct fluoroscopy at the T5 and T7 levels and then applied 5.5 x 65 mm rods, which were secured with caps screws and locked into position.
All six screws were stimulated using trigger EMGs and found to be in a safe position. We then obtained both the final AP and lateral x-rays to ensure the proper positioning of the screws. The wound was washed out copiously with bacitracin irrigation and then the high-speed drill was used to decorticate the bone and the bone chips obtained were then gathered, morselized, and used for autograft.
We also applied cancellous chips and DBX mix to create the posterior fusion mass from T5 to T7. We applied a small amount of vancomycin powder and then closed the wound in layers using #0 Vicryl sutures in the muscle. We created fascial advancement flaps over this region as it was the apex of the curve and to decrease tension on the wound.
The fascia was closed tightly with #0 Vicryl sutures and 2-0 Vicryl sutures were then used in the subcutaneous tissue followed by Monocryl at the level of the skin in a subcuticular fashion. The incision measured approximately 8.5 cm and it was dressed with Steri-Strips and an island dressing. No drains were applied. The patient was turned supine on to his stretcher and extubated without any issues. Neuromonitoring signals stayed stable throughout the case and all counts were correct at this end of the case.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

