Case Study: Cervical disc replacement in a 60-year-old female with cervical spine stenosis at C5-C6 and C6-C7 with radiculopathy and myelopathy
A 60-year-old female patient presented to our office complaining of progressively decreasing grip strength in both hands (right > left). The patient complained of increasing numbness and tingling of both the upper extremities. The is a retired school teacher who experienced a decline in the strength of both the upper extremities over the past two years.
The patient complains of neck pain and radiating pain in both arms (right > left) described as shooting down the arms. The pain is accompanied by a feeling of electrical sensation and numbness in the hands. The patient describes the clumsiness of both hands as a more recent symptom leading to severe limitation of her day-to-day activities.
Over the last two years, she had tried various conservative managements but without any significant relief. She had tried physical therapy, epidural injections, nerve root injections, and medications. She states the pain is unrelenting and disturbs her sleep.
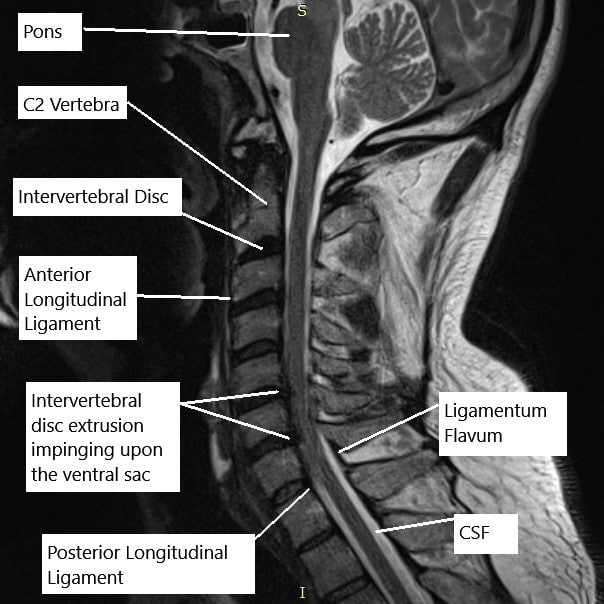
MRI of the cervical spine in the sagittal section.
The physical examination corroborated the MRI findings of the cervical spine which suggested at C5-C6, there is a posterior disc osteophyte complex. There is severe spinal canal stenosis and there is bilateral uncovertebral joint hypertrophy. There is moderate to severe right and severe left neural foraminal stenosis.
At C6-C7, there is a left paracentral disc herniation/extrusion creating impression on the ventral aspect of the thecal sac and spinal cord. There are severe associated spinal canal stenosis and bilateral uncovertebral joint hypertrophy. There is severe left-sided neural foraminal stenosis.
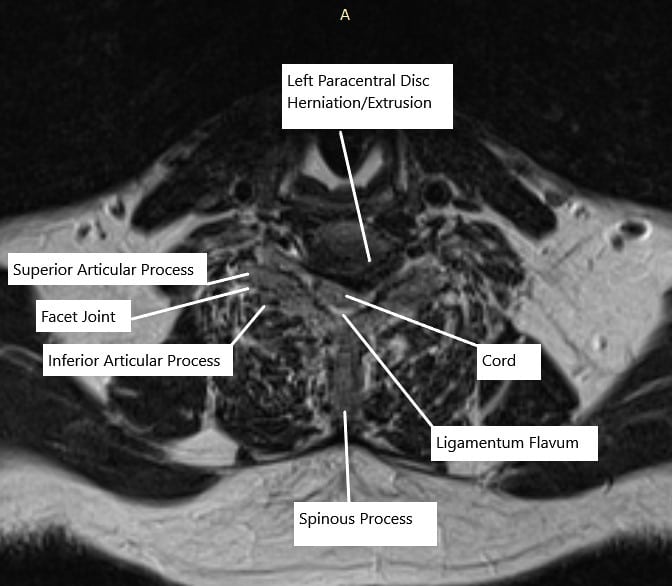
MRI of the cervical spine at C6-C7 level in axial section.
The patient was emotionally distressed at the failure of various conservative treatment options and the recent deterioration of her symptoms to the point she was not able to hold her grandson. After discussion of the risks, benefits, and various alternative treatments, the patient agreed to go ahead with surgical treatment.
PREOPERATIVE DIAGNOSIS: Cervical spine stenosis at C5-C6 and C6-C7 with radiculopathy and myelopathy.
POSTOPERATIVE DIAGNOSIS: Cervical spine stenosis at C5-C6 and C6-C7 with radiculopathy and myelopathy.
OPERATION:
- Cervical disc replacement, C5-C6.
- Cervical disc replacement, C6-C7.
- Foraminotomy and Neurolysis of Bilateral C6
- Foraminotomy and Neurolysis of Bilateral C7
- Physician directed Fluoroscopy
- Neuromonitoring
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room where general anesthesia was induced. The patient was put on the Jackson table. The neck was put in extension with the use of upper back rolls. His shoulders were taped to the table to allow fluoroscopy of the lower cervical spine. Neuromonitoring was established.
The area was cordoned and prepped and draped aseptically in the usual fashion. The preoperative antibiotic was given. A time-out was called. The right transverse approach was planned. The level was checked under lateral fluoroscopy. A transverse incision was given along the neck crease on the right side. Hemostasis was achieved and platysma was reached. Supraplatysmal dissection was performed.
The platysma was cut in the line of the incision. Supraplatysmal dissection was performed to allow mobility of the incision. With the use of Kitner, deep dissection was performed between the strap muscles and sternocleidomastoid. The anterior spine was reached. A hemostat was used to check the level and found to be at C5-C6.
Further dissection was performed distally as well as proximally to open the area. A needle was used in the disc space to confirm the level and found to be C5-C6 and saved. The disc was marked and the distal disc was also marked at C6-C7. The longus colli was raised on either side of C5, C6, and C7 to expose the body as well as the disc.
Skyline retractors were used. Caspar pin was passed into C7 and C6 to allow distraction of C6-C7. Discectomy of C6-C7 was performed using curette and Kerrison. Thorough foraminotomy of bilateral C7 was performed with the use of Kerrison punches Number 1 and 2. PLL was also excised and posterior osteophytes were removed using #1 and #2 Kerrison.
Once the discectomy was performed, the endplates were leveled. A vertebral spreader was used to check the flattening of the surface. The template was used for the disc replacement and a 19 mm x 15 mm x 6 mm disc was planned. The disc was inserted into the disc space and checked with the C-arm and found to be satisfactory.
The disc holder was removed. Now, the C7 Caspar pin was removed and inserted into C5. The distraction of C5-C6 was performed using the Caspar distractor. Discectomy was performed using a curette and Kerrison #1 mm and 2 mm. PLL was excised and osteophytes were removed.
Thorough foraminotomy of bilateral C6 was performed with the use of Kerrison punches Number 1 and 2. The disc space was sized and 6 mm x 17 mm x 15 mm disc was planned. The disc was opened, inserted into the disc space, and found to be satisfactory in the AP and lateral view of the C-arm by fluoroscopy. Finding it in a satisfactory position, the Caspar pins were removed.
The wound was thoroughly washed. Surgifoam mixed with 40 mg of Depo-Medrol was instilled into the wound to allow hemostasis. The closure was done in layers using 2-0 Vicryl for platysma, subcuticular stitch, and 5-0 Monocryl. Steri-Strip was applied over the wound. The patient was extubated and moved to recovery in stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

