Case Study: Left Total Knee Replacement
in a 68-year-old male
A 68-year-old patient presented to our office with complaints of bilateral knee pain. The patient stated that the pain started insidiously two years ago without any evident fall or trauma. The pain was especially worse in the left knee.
The pain was described as a dull ache that was not non-radiating. The intensity was moderate to severe (left greater than right). There was especially worse on activities such as prolonged walking/standing, bending, kneeling, twisting or turning.
He expressed difficulty negotiating stairs and his walking tolerance was less than a block secondary to pain. The patent also complained of stiffness about the knees after trying to get up from a chair.
He had previously consulted another physician for pain who gave him three cortisone shots in the left knee. He also tried physical therapy and heat pads but with minimal relief. Recently, the pain was so severe in the left knee, at the time he was unable to sleep.
The patient was working as an editor for a magazine and recently he had been unable to drive or sit for prolonged periods of time. He found difficulty in doing his daily activities. He was quite apprehensive about walking and used a cane as an assistive device.
He was a nonsmoker and a nondrinker. He denied any known drug allergies. His past medical history as positive for hypertension and dyslipidemia. Both his medical conditions were well controlled with medications.
On physical examination, his gait was antalgic with a reduced stance phase on the left side. There was no evidence of any genu valgum or genu varus deformity. There mild swelling with a positive patellar tap.
Tenderness was present on medial and lateral joint lines. Varus and valgus stress test was negative at 0 degrees, 30 degrees and 60 degrees. The patellar and quadriceps tendon was intact and non-tender. The anterior and posterior drawer tests and the Lachman test was negative for instability.
Pain and crepitus were present throughout the arc of motion. The range of motion ranged from 20 degrees to 100 degrees. There was a 20 degree fixed flexion deformity. The examination of the right knee revealed similar findings. The examination of the bilateral hips and ankles was normal.
The bulk and tone of the bilateral lower limb muscles were normal. The neurological examination of the lower limbs revealed no deficit. The bilateral lower extremity pulses were palpable and comparable.
Imaging studies revealed severe bilateral osteoarthritis. The left knee was worse than the right knee. Considering the patient’s lifestyle limiting knee pain, he was advised left total knee replacement. Risks, benefits, and alternatives were discussed at length with the patient and his son. He decided to go ahead with the procedure.


Preoperative X-ray of the left knee showing severe osteoarthritis in anteroposterior and lateral views.
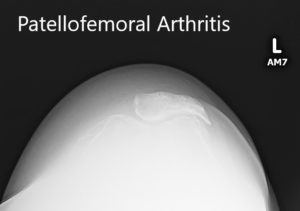
Preoperative X-ray showing the merchant view of the patella with severe patellofemoral arthritis.
OPERATION: Left total knee arthroplasty.
IMPLANTS USED: 52-mm all-poly patella with size 6 femur with size E stemmed tibia with 14-mm stem extension.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent, signing on the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient as well as with the son prior to the procedure.
The patient was brought to the operating room, and the tourniquet was placed over the left thigh. The left lower extremity was then draped and prepped in the usual sterile manner after anesthesia was obtained. A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were then incised.
Medial parapatellar arthrotomy was then performed. The knee was then exposed. The femur was then exposed and the distal cutting guide was then placed into position after making drill holes in the femoral canal. The distal cut was then performed. The anterior, posterior, and Chamfer cuts were then performed.
Attention was then turned towards the tibia. The tibial cut was then performed. The tibia was then broached. The femur was then resected for the notch. Medially and laterally meniscus was debrided. The cruciates were then debrided. Gap balancing was then performed. Gap balancing was perfect.
The trial femur was placed into position followed by the trial tibia and the poly. The patellar resection was then performed. The trial patella was then placed and the knee was trialed through a range of motion. The 20-degree fixed flexion deformity no longer existed.
The full flexion was obtained. The trial components were then removed. Cement was mixed. Thorough lavage was given. The bone was then dried. The femur was cemented into position followed by the tibia. The poly was then placed into position. Excess cement was removed. The knee was then reduced and then held in full extension with a bump under the ankle.
The patella was instrumented into position and held with a patellar clamp. After the cement hardened, the patellar clamp was removed. Everstill was used. The injection was given for periarticular pain relief.
The medial parapatellar compartment was closed with Ethibond and Quill. Subcutaneous tissues were closed with O Vicryl. Subcuticular tissues were closed with 2-0 Vicryl. The skin was closed using staples. Sterile dressing was applied to the wound, and the patient was transferred to the postoperative care unit in a stable condition.
The limb was exsanguinated and the tourniquet was elevated prior to the incision, and after the incision, the tourniquet was let down. The patient was then transferred to the postoperative care unit in a stable condition.


Postoperative X-ray showing the left knee joint with prosthesis in anteroposterior and lateral views
The patient had a good recovery post-op with stable vitals. He was able to walk with support the same day of the surgery. His calves were soft and non-tender with Homan sign negative. The pain was well controlled with medications.
He was prescribed aspirin for deep vein thrombosis prophylaxis. Physical therapy was initiated for increasing strength and flexibility. The sutures were removed post-op day 15 with no complications. The wound was clean, dry and had healed well.
Twelve weeks post-op, he was walking without any support totally pain-free. He had a full range of motion and continued a home exercise program. He was back at his job and expressed satisfaction with the outcome. He reported decreased pain in the right knee secondary to offloading.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

