Case Study: Customized Total Knee Replacement in a 58-year-old female with Arthritis
A 58-year-old female presented to our office complaining of worsening right knee pain. She first noticed the pain 10 years ago after a twisting injury during hiking. She stated she was diagnosed with a torn meniscus. She underwent a meniscal repair arthroscopic surgery with an outside physician.
She reported the pain initially got better after the surgery but returned gradually a few months after the operation. She describes the pain as a dull ache, greater on the inner side of the knee. The pain was especially worse after activities such as going up the stairs or bending the knees.
Recently, the pain had gotten worse for the past 1 year limiting her daily activities. She finds it increasingly difficult to walk more than 2 blocks and performing activities involving bending, kneeling or sitting for a long time. She is a retired teacher currently volunteering at a hospital.
The patient was an active smoker (10 pack-years) with a medical history of coronary artery disease (CAD), dyslipidemia, and varicose veins. Her surgical history involved a stented coronary artery and an endovenous laser ablation of left greater and lesser saphenous veins.
She previously had knee injections in the form of hyaluronic acid and cortisone. She described brief relief from symptoms that didn’t last for more than 5 weeks. She also tried other conservative management in the form of physical therapy and heat pads but with no relief.
The patient was visibly anxious and distressed about the pain affecting her lifestyle. She described getting apprehensive about carrying out her daily activities secondary to pain. She stated not being active made her emotionally vulnerable.
Her physical examination revealed mild swelling in the right knee with no erythema or rise of temperature. There was a medial joint line and medial patellar facet tenderness. The range of motion was full with no deformity. There was no distal neurological deficit. The examination of her bilateral ankles and knees was unremarkable. Her imaging studies revealed severe tricompartmental osteoarthritis of the right knee.
The patient was given a smoking cessation education which she was motivated to quit smoking. Her current medications included Vasotec, simvastatin and aspirin. After careful consideration of her lifestyle limiting knee pain and comorbidities, she was advised a custom total knee replacement.
Risks, benefits and potential complications especially being a high-risk patient due to CAD and smoking were discussed in-depth with the patient. She agreed to go ahead with the procedure.
A preoperative CT scan of the right knee with the hip and ankle was taken several weeks prior to the procedure. This aided in a better understanding of the patient’s knee anatomy and biomechanics. The data was used to construct a patient-specific implant. Disposable cutting blocks were constructed for creating bone resection as outlined in a preoperative surgical plan.


Preoperative weight-bearing X-ray showing AP and lateral views of the right knee
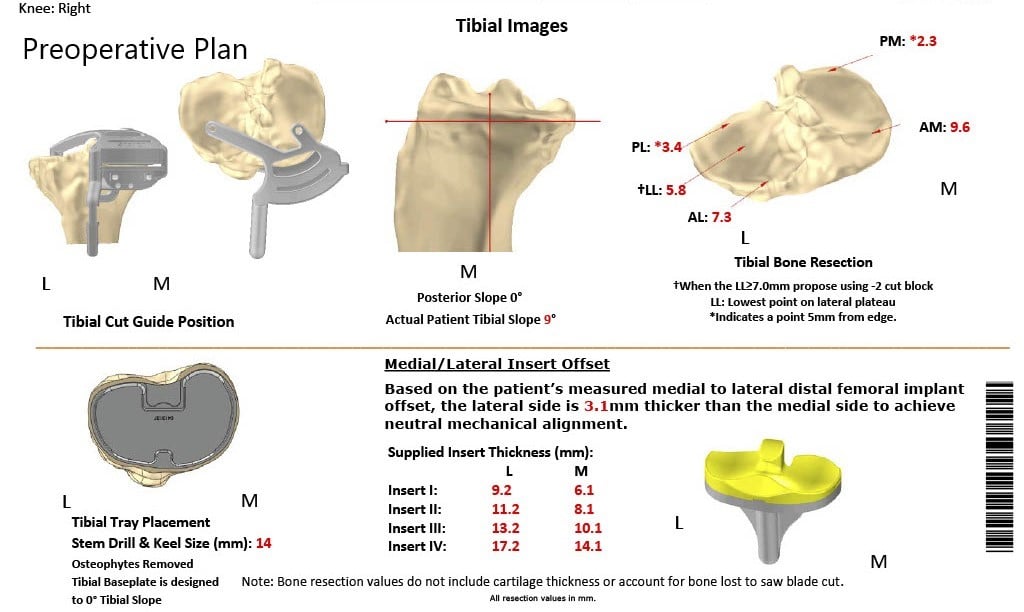
Complete Orthopedics patient-specific surgical plan for a customized total knee replacement in a 58-year-old female with arthritis.
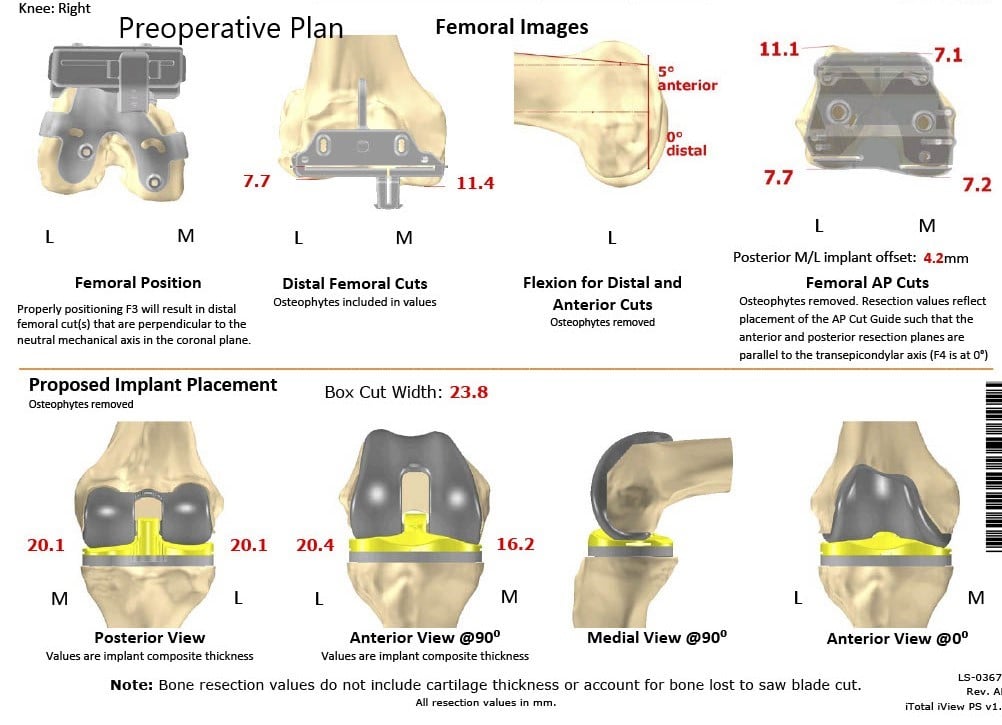
Complete Orthopedics patient-specific surgical plan for a customized total knee replacement in a 58-year-old female with arthritis (scan 2)
A preoperative surgical plan outlining the bone cuts and femoral offsets
Operative report:
The implant used: Custom femoral implant with a custom tibial tray with a 6 mm polyethylene insert and 32 mm x 8.5 mm patella.
Description of procedure: The patient was brought to, the operating room after obtaining informed consent and signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure.
Anesthesia was obtained by the anesthesiologist. The patient was then definitively positioned and the tourniquet was used to exsanguinate the extremities. A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised. Medial parapatellar arthrotomy was then performed. The tibial cutting guide was used to make the tibial cut and the tibia was then prepared.
Attention was then turned on towards the femur. The femoral cutting guides were used for preparing the femur and then medially and laterally, laminar spreaders were then used and the remainder of the cruciates and the meniscus were then debrided. Gap balancing was performed and found to be perfect.
The patella was resected. Drill holes were made in the patella. The trial patella was placed into position followed by a trial of the femur, trial tibia, and the polyethylene was then placed over the tibia.
The knee was reduced and trialed through a full physiological range of motion and excellent stability and excellent patella tracking was then observed. The trial components were then removed.
The injection was given. A thorough lavage was given. The femur was cemented into position. Excess cement was removed. The tibia was cemented into position. Excess cement was removed.
Poly was then placed over the tibia and the knee was reduced and held in full extension with a bump under the ankle. Patella was then cemented into position and held with a patellar clamp.Medial patellar arthrotomy was closed with Vicryl and Stratafix. The wound was closed in layers. Sterile dressing was then applied over the wound. The tourniquet was then let down, and the patient was transferred to the postoperative care unit in stable condition.


Postoperative X-ray of the patient showing AP and lateral views of the right knee
The post-operative recovery was excellent with only complains of pain which was well managed with pain medications. She was able to walk with support on the same day of surgery. Postoperative day 15 her staples were removed and the wound was dry, clean and healed. She continued motivated not smoking and was happy with the outcome of the surgery.
Physical therapy was initiated to regain muscle strength and improve flexibility. She complained of some stiffness for which cold therapy and continuous passive motion therapy was started. After three months she had successfully concluded her physical therapy and reported no pain in the right knee. She had since returned to volunteering at the hospital and was more active socially secondary to her increased mobility.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

