Case Study: Bilateral Customized Total Knee
Replacement in a 72-year-old female
A retired home health aid presented to our office with complaints of bilateral knee pain for the past 2 years. She didn’t recall any precipitating factors leading to pain but felt her long career as a health aid for 40 years contributed to her knee pain.
She described the onset of knee pain as insidious located on the inter sides if both knees (right greater than left). The pain was described as a sharp pain occurring constantly. The pain was exacerbated by activities such as prolonged walking, standing, turning, twisting, kneeling and bending.
She found it difficult to navigate stairs secondary to pain. Her current walking capacity was limited to 3 blocks due to pain. Recently, she expressed dismay at the inability to even die daily activities such as cooking, doing her laundry and cleaning the house.
She was currently living with her daughter and was distressed by not being able to spend quality time with her family. She reported disturbed sleep due to pain. The intensity of pain was described as 7/10 on a scale of 0 to 10. She had planned to volunteer at a hospital for children but was unable to do so due to pain.
She previously had a meniscal surgery done on both her knees a year ago. She reported that the relief lasted only for a month. She also tried conservative management options such as physical therapy, cortisones knee injections, and heat pads, but with minimal relief.
She was an active smoker, smoking one cigarette every day down from half a pack 20 years ago. She was currently taking Simvastatin 20 mg for dyslipidemia and Vasotec 10 mg for high blood pressure. She had a surgical history of hysterectomy 20 years ago and a renal stone removal 12 years ago.
On physical examination, her gait was steady and she used a cane for ambulation. There was genu varum deformity in both knees. The skin overlying both the knees was normal. There was mild swelling in bilateral knees, the patellar tap was positive on milking the suprapatellar pouch. Tenderness was present on the bilateral medial joint and lateral joint line.
There was tenderness on bilateral patellar facets and crepitus was present on the range of motion of both knees. The range of motion of both the knees was painful terminally. There was no fixed flexion or extension deformity. On testing for instability, there was no evidence of coronal, sagittal or rotational plane laxity/instability.
Imaging study revealed severe osteoarthritis of both knees. Considering her lifestyle limiting knee pain, she was offered bilateral custom total knee replacement. Risks, benefits, and alternatives were discussed thoroughly with her and her daughter. She agreed to go ahead with the surgery.

Preoperative X-ray showing the AP view of both the knee joints.


Preoperative X-ray showing the lateral view of the left and the right knee joint.
As a part of preoperative planning, a CT scan of the lower extremities was obtained. The data obtained was used to analyze the correct biomechanics and anatomy of the knees. Customized disposable instruments and cutting blocks were made to aid in the surgery. Patient-specific implants were constructed to match the patient’s anatomy. A preoperative plan was formulated to guide the surgical steps.

Complete Orthopedics patient-specific surgical plan for a bilateral customized total knee replacement in a 72-year-old female.
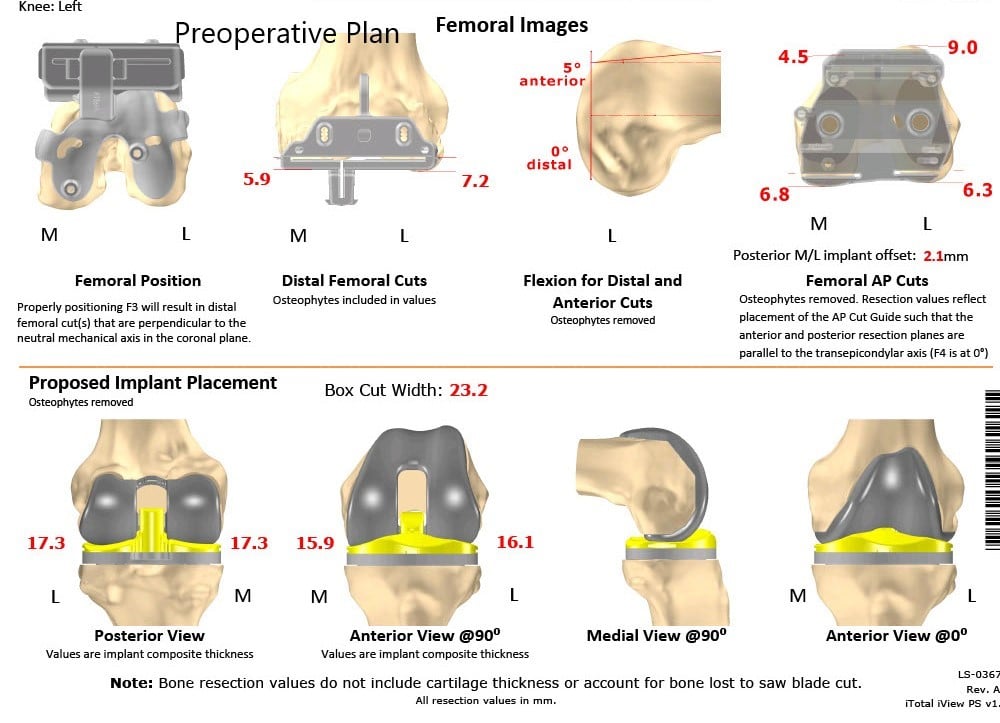
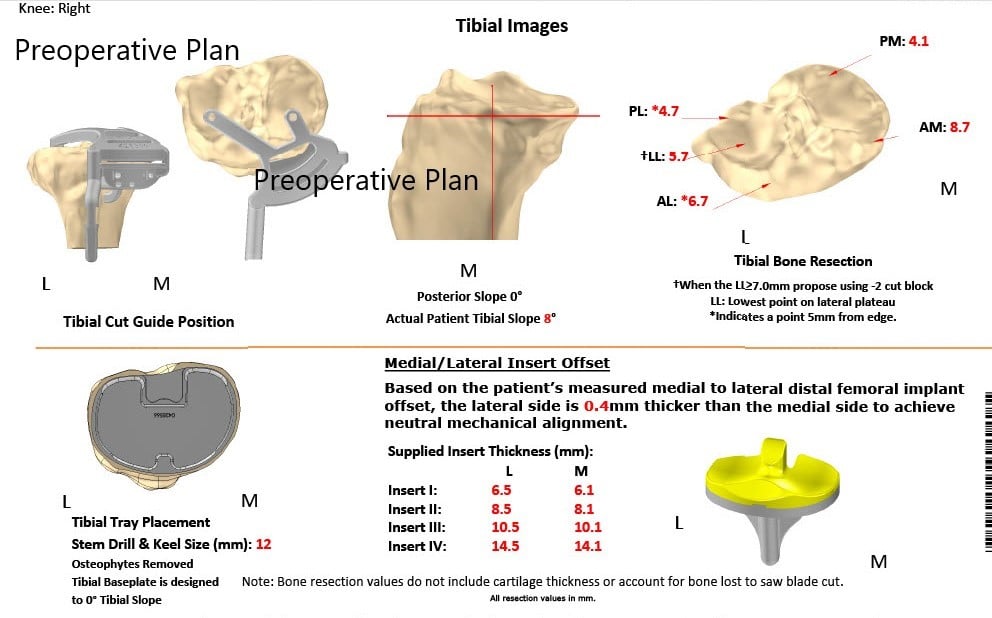
Complete Orthopedics patient-specific surgical plan for a bilateral customized total knee replacement in a 72-year-old female (scan 2)
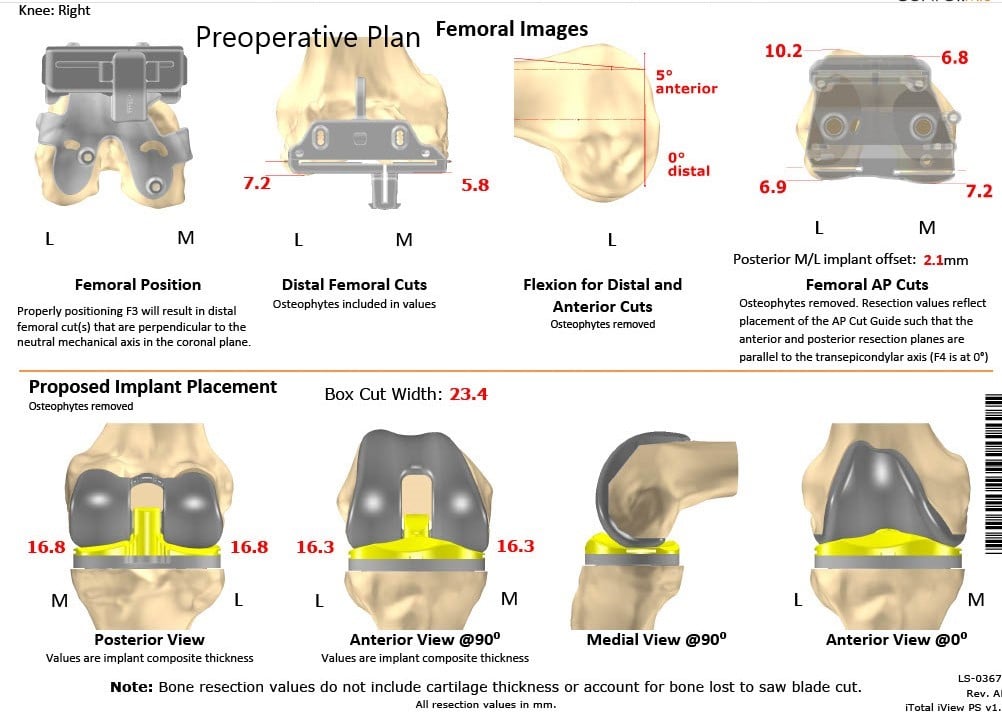
Complete Orthopedics patient-specific surgical plan for a bilateral customized total knee replacement in a 72-year-old female (scan 3)
Complete Orthopedics patient-specific surgical plan for a bilateral customized total knee replacement in a 72-year-old female (scan 4)
OPERATION: Bilateral total knee arthroplasty, right total knee replacement, followed by a left total knee.
IMPLANTS USED: Customized femoral and tibial implants.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent, signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient understands the increased risks associated with bilateral knee replacement surgery.
The patient was brought to the operating room. Anesthesia was obtained by the anesthesiologist. The patient was then definitively positioned, and both knees were then draped in the usual sterile manner. Esmarch was used to exsanguinate the limb on the right side, and the tourniquet was elevated.
Skin and subcutaneous tissues were incised. The fascia was then divided. A medial parapatellar fasciotomy was performed. The tibia was exposed, and a tibial cutting guide was placed into position. The tibial cut was performed.
Attention was then turned towards the femur. The anterior, posterior, and chamfer cuts were then performed using the femoral cutting guide. Lamina spreaders were used medially and laterally, and the remainder of the meniscus was debrided.
Posterior osteophytes were then removed. Gap balancing was performed and was found to be correct. Attention was then turned towards the patella. The patellar resection was performed. Drill holes were made in the patella. The trial patella was then placed into position. The osteophytes were removed. 
The femoral component was then placed into position. The tibial component was placed into position. Poly was placed into position. The knee was reduced and then trialed through a full range of motion. Excellent patellar stability was observed, and full extension and full flexion were possible intraoperatively.
The trial components were then removed. Thorough lavage was given. The injection was given. The femur was cemented into position, followed by the tibial. Poly was placed into position, and the knee was reduced.
Excess cement was removed. The knee was held in full extension, and the poly was then cemented over the patella and was held in position with a patellar glide.
After the cement hardened, the clamp was removed. Thorough lavage was given. Medial parapatellar arthrotomy was closed with O Vicryl and with Quill. Cutaneous tissue was closed with O Vicryl.
Subcuticular tissue was closed with 2-0 Vicryl. The skin was closed using staple s. Sterile dressing was applied over the wound, and attention was then turned towards the left knee.
After the tourniquet was let down on the right side, the tourniquet was elevated on the left side. Skin and subcutaneous tissues were incised. Medial parapatellar arthrotomy was performed. Attention was then turned towards the tibia. Tibial resection was performed, followed by the femoral resection. Lamina spreaders were used medially and laterally, and the remainder of the cruciates was then divided.
Attention was then turned towards the patella. The patellar resection was performed. Drill holes were made in the patella. The trial patella was placed into position. Osteophytes were removed.
Attention was then turned towards the femur. The trial femur was placed into position, followed by the trial tibia. Poly was placed into position. The knee was then balanced through a full physiological range of motion. Excellent patellar stability was achieved. Full-extension was achieved. Full flexion was achieved.
Trial components were then removed. The injection was given. Thorough lavage was given. The femur was cemented into position. Excess cement was removed. The tibia was cemented into position. Excess cement was removed. Poly was placed into position.
The knee was reduced and held in full extension with a bump under the ankle. Patella was cemented into position. Excess cement was removed. Patella was held in position with a patellar glide.
After the cement hardened, the patellar clamp was removed. A lavage was given. Medial parapatellar arthrotomy was closed with 0 Vicryl and with Quill. Cutaneous tissue was closed with O Vicryl. Subcuticular tissue was closed with 2-0 Vicryl. The skin was closed using staples. Sterile dressing was applied over the wound. The patient was then transferred to the postoperative care unit in stable condition.

Postoperative X-ray showing the AP view of both knees.


Postoperative X-ray showing the lateral view of the right and the left knee.
Post-op the patient was walking the same day of surgery with support. Thrombotic-event-deterrent (TED) stockings were advised to the patient along with aspirin for deep vein thrombosis prophylaxis. The patient’s pain was managed well with medications.
Sutures were removed the 14th-day post-op uneventfully. The patient reported zero pain at the two months follow up. She was walking without the support and had a full range of motion of both knees. She was extremely happy with the outcome. She follows up as needed.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

