Case Study: Bilateral Custom Total Knee Replacement
in a 61-year-old male with Knee Arthritis & Genu Valgum Deformity
The patient was a 61-year-old man presenting with complaints of bilateral knee pain. He first noticed the pain while walking on the beach two years ago. The pain was located along the inner sides of both knees. The patient denied any precipitating injury or fall leading to knee pain.
The pain was described as sharp pain and moderate to severe in intensity. The pain was exacerbated on activities such as walking, sitting and getting up from a chair, navigating stairs, bending, and kneeling. The patient denied any laxity or instability in the knee. There was no radiation of the pain.
The patient previously consulted another physician who gave him gel injections in both knees. He reported relief for only two weeks. He subsequently received cortisone injections in both knees without significant relief. He had tried physical therapy and heat therapy without much help.
He was a nonsmoker and nondrinker and had a family history of hip and knee arthritis. He was currently taking Lipitor for dyslipidemia and Flomax for benign hypertrophy of the prostate. He stated he was prediabetic but was unable to exercise or walk secondary to knee pain.
He was a librarian and currently not working due to pain. His work involved lifting, moving and walking around the aisles of the library. He stated feeling bad not being able to go to the library and interact with people, a career he had pursued passionately for the past 45 years.
On physical examination, there was genu valgum deformity in both knees. The gait of the patient was steady and coordinated. The skin overlying both the knees was normal with no evidence of any scar marks or sinus tracts. There was the presence of mild swelling in both knees demonstrated on milking the suprapatellar pouch.
There was tenderness on bilateral medial and lateral joint lines and patellar facets. The range of motion was restricted secondary to pain in both knees (right- 5 degrees to 90 degrees, left- 10 degrees to 80 degrees). There was no evidence of any laxity or instability in coronal, sagittal and axial planes.
The examination of bilateral hips revealed bilateral hip bursitis. The examination of the bilateral ankle was normal. There was no distal neurological deficit and the bilateral pulses were palpable and comparable. There was no bowel or bladder dysfunction. The bilateral lower extremity deep tendon reflexes were present and comparable.
Imaging studies done revealed severe tricompartmental osteoarthritis in both knees. Considering his lifestyle limiting knee pain and exhaustion of conservative management options, he was advised bilateral knee replacement. He was deemed a candidate for custom total knee replacement. He agreed with the plan.
As a part of the preoperative assessment, a CT of both the knees with hips and ankles was obtained a couple of weeks prior to the procedure. Anatomical and biomechanics assessment was done for constructing custom implants. Further, disposable bone cutting jigs were made customized for the patient’s knees. A preoperative plan was made outlining the steps and bone cuts.


Preoperative X-ray showing the AP view of the left and the right knee respectively.


Preoperative X-ray showing the lateral views of the right and the left knee respectively.
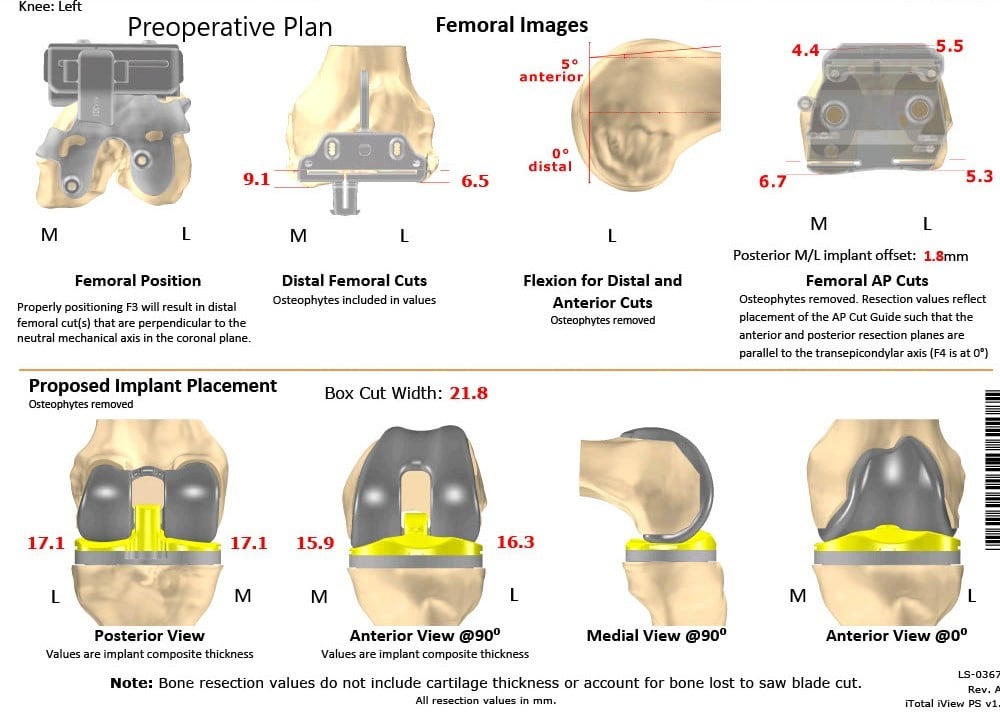
Complete Orthopedics patient-specific surgical plan for a bilateral custom total knee replacement in a 61-year-old male with knee Arthritis & Genu Valgum Deformity.
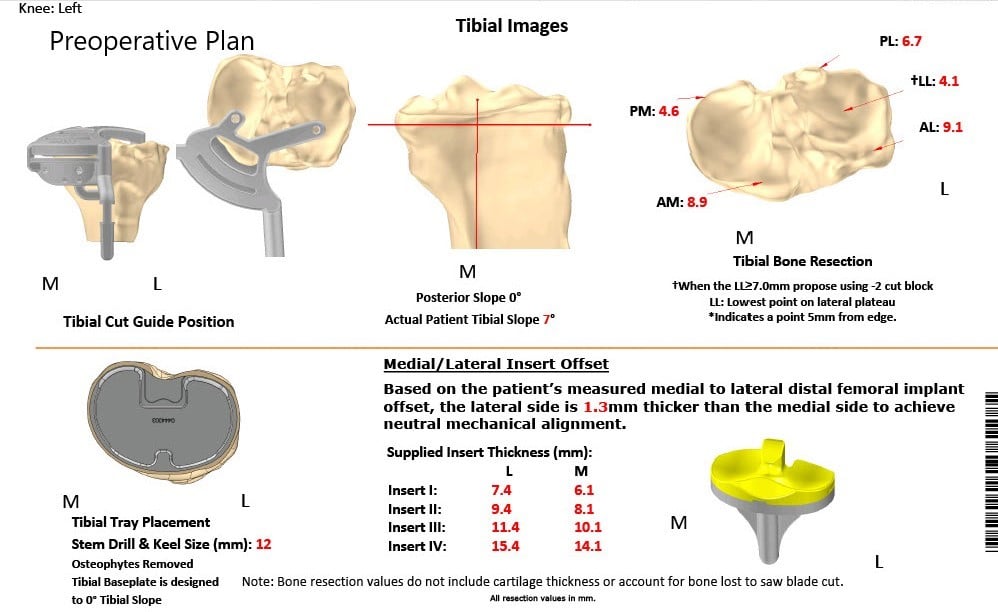
Complete Orthopedics patient specific surgical plan for a bilateral custom total knee replacement in a 61-year-old male with Knee Arthritis & Genu Valgum Deformity (scan 2)
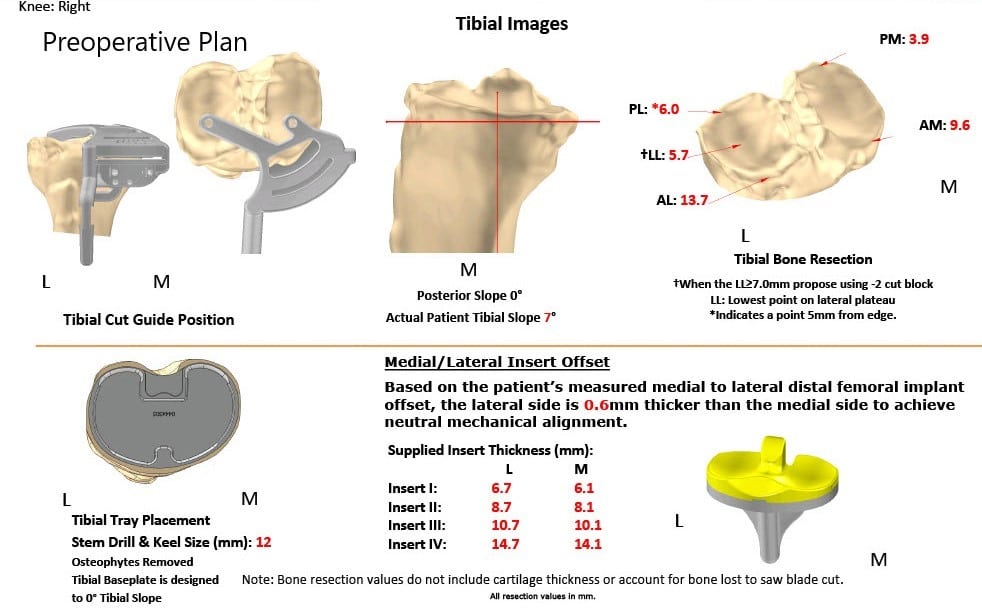
Complete Orthopedics patient specific surgical plan for a bilateral custom total knee replacement in a 61-year-old male with Knee Arthritis & Genu Valgum Deformity (scan 3)
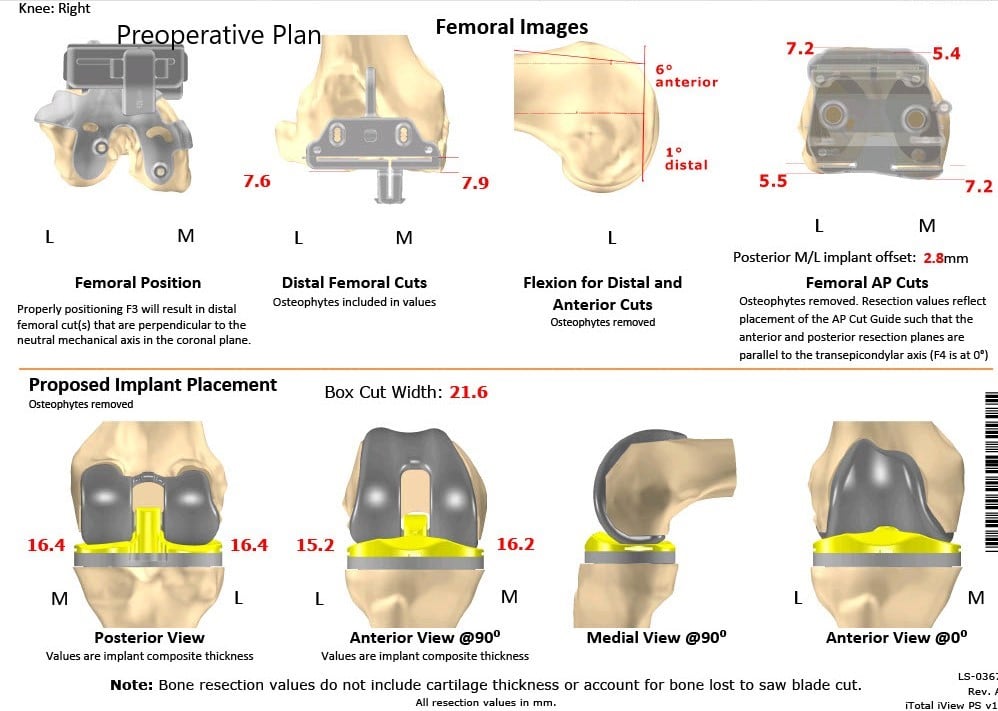
Complete Orthopedics patient specific surgical plan for a bilateral custom total knee replacement in a 61-year-old male with Knee Arthritis & Genu Valgum Deformity (scan 4)
OPERATION: Bilateral total knee arthroplasty.
IMPLANTS USED: Custom tibial tray with a Custom femoral implant with a custom patella implant 29 mm with 8-mm polyethylene insert on the left side, and with a 6 mm polyethylene insert with poly 32 mm x 6 mm patellar implant with a custom femoral implant with a custom tibial tray.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room. After obtaining informed consent, signed the correct surgical site, the risks, benefits, and alternatives were extensively discussed with the patient and with the family prior to the procedure.
They understood the increased risk of bilateral total knee replacement.
It was decided to do the left knee first because the left knee was more symptomatic than the right. Both knees were then draped and prepped in the usual sterile manner.
An Esmarch was used to exsanguinate the limb and the tourniquet was elevated. A straight incision was used for arthrotomy. Skin and subcutaneous tissues were incised.
Medial parapatellar arthrotomy was then performed. The tibia was then subluxated and the tibial preparation was then performed. A tibial cut was used making the custom tibial guide. The bone was then removed. The tibia was then prepared.
Attention was then turned towards the femur. The femoral custom guides were used for making the distal chamfer as well as the notch cut. The laminar spreaders were used medially and laterally and the osteophytes were then removed. Gap balancing was performed, and the gap was well balanced.
The patella was then resected. Drill holes were then made in the patella. The trial femur was then placed into position followed by the trial tibia and the poly. The knee was then trialed through a full physiological range of motion. There was a full-extension, full flexion possible. The patellar tracking vas excellent.
Trial components were then removed. The injection was given in the knee. A thorough lavage was given. The femur was cemented into position. Excess cement was removed. The tibia was then cemented into position. Excess cement was removed. The poly was then placed on the tibia and the knee was then reduced.
The knee was held in full extension with a bump under the ankle and the patella was then cemented into position. Patella was held in position with a patellar clamp. Excess cement was removed. Thorough lavage was given.
Medial parapatellar arthrotomy was closed with 0 Vicryl in Stratafix, cutaneous tissues were closed with 0 Vicryl, subcuticular tissues were closed with 2-0 Vicryl, the skin was closed using staples. The tourniquet was let down. Sterile dressing was then placed over the left knee.
Attention was then turned towards the right knee. Esmarch was used to exsanguinate the limb. The tourniquet was then elevated. A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were then incised. Medial parapatellar arthrotomy was then performed.
The tibia was then subluxed and the tibia was then prepared. The tibial resection was made using the custom guide. Attention was then turned towards the femur. The femur was then prepared and the custom guides were used for the distal chamfer as well as the notch cuts.
The medial and lateral laminar spreader was used for debriding the meniscus and the posterior osteophytes were then removed. Gap balancing was performed, and the gap was well balanced.
The patellar resection was then performed. Drill holes were then made in the patella. The trial patella was then placed into position, followed by the trial femur and the trial tibia. Trial poly was then placed into position.
The knee was then trialed through a full physiological range of motion. Full-extension was achieved, full flexion was achieved, patellar tracking was excellent. Trial components were then removed. Thorough lavage was given. An injection was given. Femur was cemented into position followed by the tibia.
The final poly was then placed into position. The knee was then reduced and held in full extension with a bump under the ankle. Thorough lavage was given. The patella was then cemented into position and was held with a patellar clamp. Excess cement was removed. Thorough lavage was given.
After the cement hardened, medial parapatellar arthrotomy was closed with Vicryl and with Stratafix. Cutaneous tissues were closed with O Vicryl, subcuticular tissues were closed with 2-0 Vicryl, the skin was closed using staples.
Sterile dressing was then applied to the wound. The tourniquet was let down. The patient was then transferred to the postoperative care unit in stable condition.
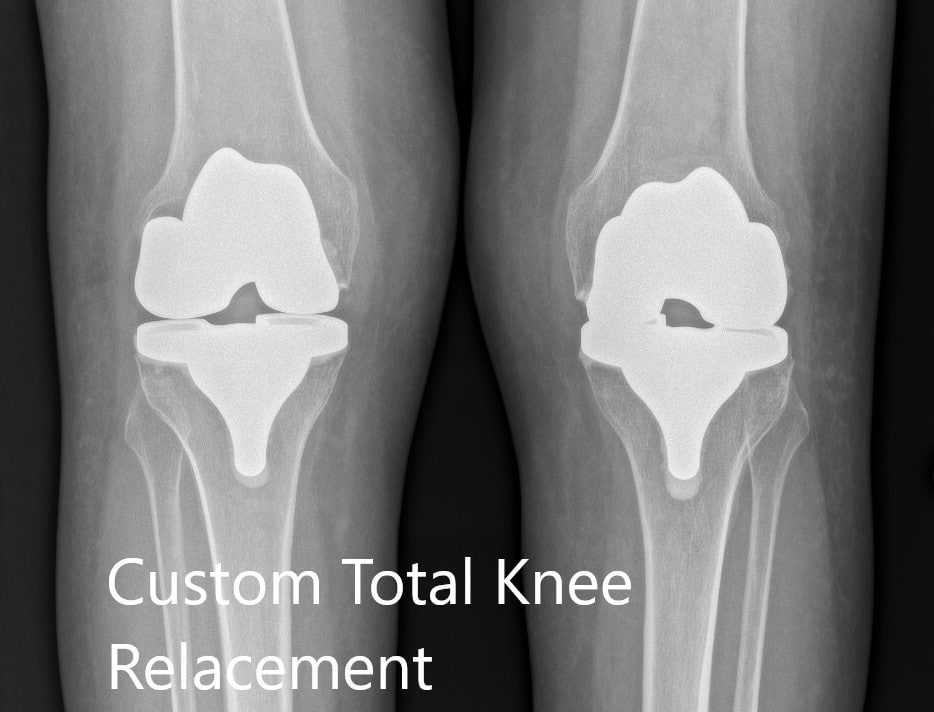
Postoperative X-ray showing the AP view of both knees.


Postoperative X-ray showing the lateral view of the right and the left knee respectively.
The patient was able to walk the same day of the procedure. He felt confident and comfortable walking. His post-op pain was managed well with medications. He was prescribed medications (aspirin) for deep vein thrombosis prophylaxis. Physical therapy was started to increase range of motion and strengthen the muscles.
The sutures on both knees were inspected to be clean, dry and intact. Three months post-op the patient was happily walking without support. He reported zero pain and demonstrated a full range of motion. He was happily back to do his daily activities and enjoyed his job as a librarian. He follows up as needed.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

