Case Study: Total Hip Replacement in a 52-year-old male with
Avascular Necrosis (AVN) of the Left Hip with prior Hip Dislocation
A 52-year-old male presented to our office with complaints of left hip pain and stiffness for the past 6 years. He had a history of traumatic hip dislocation 7 years ago. The patient was involved in a skiing accident leading to left hip dislocation. The patient was airlifted from the remote location to a nearby hospital. The reduction was achieved under anesthesia after 6 hours post dislocation.
He subsequently had an abduction brace worn for a month. The patient gradually returned to full physical activity. He first noticed the hip pain a year after the accident while hiking at a trail. The pain gradually worsened to the point he was unable to walk unassisted. He currently used a cane as an assistive device.
He earlier saw another physician who prescribed him bisphosphonates and blood thinners. He was a nonsmoker, nondrinker and had no known drug allergies. He was not suffering from any other medical condition. He denied any childhood hip surgery or infections.
The pain was moderate in intensity located in the left groin. There was no radiation of the pain and character was reported as a dull ache. The pain was worse on activities such as bending, squatting, getting up from a chair and walking. His walking capacity was limited to less than 5 blocks.
He was currently not working and was previously employed in a travel agency. He loved to travel and go on hikes, a hobby unfortunately he was no more able to pursue. He was living with his wife and two children and was distressed with the lifestyle limitations. He was no longer able to perform daily activities with ease. The pain disturbed his sleep and he reported anxiety during the daytime.
On physical examination, he walked with an antalgic gait. The stance phase of the gait was reduced on the left side. There was no exaggeration of the lumbar lordosis. There was no structural or functional scoliosis. Both the shoulders, iliac spines, patella, and the malleolus were are the same levels.
On the supine examination, both the anterior superior iliac spines were at the same level. There was no swelling in the left groin. The skin overlying the left groin was normal with no evidence of scar marks or sinus tracts. The greater trochanter was normal with no tenderness or broadening/thickening.
There was a left leg length shortening of 1 cm on the measurement of both true and apparent lengths. There was no fixed adduction, internal rotation, or flexion deformity. The range of motion was painful, especially on rotational movements. There was a differential rotation on the left hip on flexion (sectoral sign). The limitation of left hip internal rotation and abduction was marked.
The bulk and tone of the left lower extremity were normal. There was no wasting of the gluteal or the thigh muscles. The examination of the right hip, bilateral knees, and ankles were normal. There was no distal neurological deficit. The bilateral lower extremity pulses were palpable and comparable.
Routine blood investigations were performed and an X-Ray of the pelvis work both hip bones was obtained in the anterior-posterior and lateral views. There was marked left hip joint space destruction. The contour of the left head of the femur was nonspherical. There was marked sclerosis and subchondral cysts. Avascular necrosis of the hip joint was suspected.

Preoperative X-ray of the pelvis with both hips in anteroposterior view.
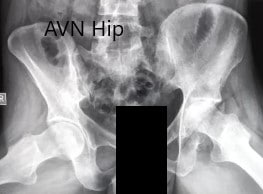
Preoperative X-ray of the pelvis with both hips in frog-legged lateral views.
An MRI of the pelvis was obtained which suggested decreased signal intensity on both T1WI and T2WI suggesting sclerosis and periarticular edema. There was a collapse of the head of the femur. The features were suggestive of advanced avascular necrosis of the left hip joint.

MRI showing the T1WI of the pelvis.

CMRI showing the T2WI of the pelvis.
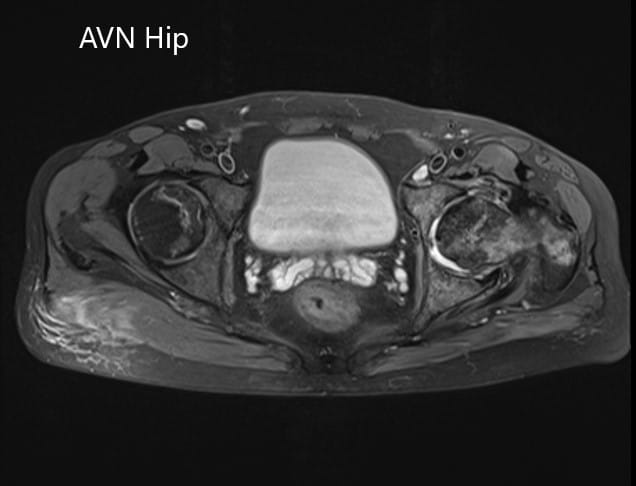
Axial section of the T2WI of the pelvis.
The patient had advanced avascular necrosis of the left hip with collapse and acetabular changes. There was a positive history of prior traumatic hip dislocation. Considering lifestyle limiting hip pain and advanced avascular necrosis, the patient was advised a left total hip replacement. Risks, benefits, and alternatives were discussed with the patient and his wife.
The patient agreed to undergo the procedure. He underwent a left total hip replacement. The bone biopsy obtained during the procedure was sent for pathological analysis. The report came positive for avascular necrosis of the head of the femur with ischemia of the marrow.
He was started on pain medications and aspirin for deep vein thrombosis prophylaxis. The stitches were removed 15th-day post-op without any complications. Hip precautions were explained to the patient.
The patient was quickly able to return to his baseline activities in 10 weeks. He was able to walk without support and reported no pain. He had an excellent range of motion of the left hip. He was able to drive his car, do his laundry, walking his dog and carry on all his daily activities with ease.
He was extremely happy with the outcome and planned to go hiking in three months.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

