Case Study: Right Total Hip Replacement
in a 75-year-old female
A 75-year-old female presented to our office with complaints of right hip pain for the past 2 years. She reported that the pain was insidious in onset. The pain was located on the right groin radiating to the right knee. She describes the pain as a dull ache which was moderate in intensity (6/10). The patient states the pain has gradually worsened for the last 2 years.

Preoperative X-ray of the pelvis, AP view, and frog-legged lateral view of the right hip.
The patient was fit and active currently running a flower shop as a florist. Her work demanded her to bend, walk and go up and down the stairs. She loved riding a bicycle in the evenings, a hobby she was no longer able to pursue due to pain.
She was a former smoker with no known drug allergies. Her comorbidities included asthma, hypertension and gastroesophageal reflux disease. All her comorbidities were well controlled with medications.
He denied the use of any anticoagulants or immunosuppressants. She denied any history of alcohol abuse, steroid intake, previous trauma, low back pain and stiffness in the neck, multiple joint pain or epilepsy.
She reported a crunchy feeling described as bone rubbing against the bone on bending or getting up from the chair. Recently she was finding it difficult to perform daily activities such as putting on her socks. The patient also reported stiffness in the right hip after sitting for a prolonged period of time.
Previously, the patient had tried a myriad of conservative treatment options such as physical therapy, heat and massage, range of motion exercises, and medications.
She reported no long term relief of symptoms from the aforementioned conservative management. She was currently using a cane as a walking aid to offload the right hip.

Preoperative X-ray of Pelvis AP view and frog-legged lateral view of the right hip (image 2)
Her physical examination revealed a bipedal, stable, coordinated, antalgic gait with reduced stance phase on the right side.
On supine examination, there was no exaggerated lumbar lordosis and both her anterior superior iliac spines (ASIS) were at the same level. There were no skin scars and sinuses or any fullness in the scarpa’s triangle
There was no leg length discrepancy and no muscle wasting. On deep palpation, there was positive tenderness over the anterior joint line on the right hip.
There was no thickening, broadening or tenderness over the trochanter. The range of motion was full with painful end extension and abduction. There were no deformity in the sagittal, coronal or axial planes.
Imaging study revealed right hip osteoarthritic degeneration. After taking her comorbidities and lifestyle limiting right hip pain into consideration, she was advised right total hip replacement. Risks, benefits, and alternatives were discussed with her at length. She agreed to go ahead with the procedure after medical clearance.
Operative report: Right total hip arthroplasty
Implants: Acetabular Shell 52 mm with 0-degree polyethylene insert 36 mm with a 6.5-mm screw with a 36-mm ceramic femoral head with a size 7, 127 degrees Femoral Prosthesis (114mm).
Description of procedure: The patient was brought to the operating room after obtaining informed consent and signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was definitively positioned with the right hip up, and the right hip was then draped and prepped in the usual sterile manner.
A curved incision centered over the greater trochanter was used for the arthrotomy. Skin and subcutaneous tissues were incised. The fascia was then divided. The hip was then placed in extension and internal rotation, and the posterior soft tissue structures were then taken down and tagged for future repair.
The hip was then dislocated, and the neck resection was made at the correct level after measuring the lesser trochanter to the center distance and comparing with the preoperative radiographs.
Attention was then turned towards the acetabulum. There were significant osteophytes that were removed. Acetabulum exposure was achieved. The acetabulum was then debrided. The acetabulum was then sequentially reamed.
The final shell was then placed into position in the correct abduction and anteversion. The screw was used for additional fixation. A poly was then placed over the shell. Additional osteophytes were then removed.
Attention was then turned towards the femur. The femur was then sequentially broached. The final broach was left into position. The trunnion and the head were then placed over the broach.
The lesser trochanter to the center distance was then measured and was found to be correct. The hip was then re-located and trialed through a full physiological range of motion. The hip was stable in a physiological range of motion.
The hip was then dislocated. Trial femur Mas then removed. The final prosthesis was then placed into position. The hip was then reduced again. Thorough lavage was given. In injection was given. Posterior soft tissue structures were then tagged to the greater trochanter through transosseous tunnels.
The fascia was closed with Vicryl. Cutaneous tissues were closed with O Vicryl. Subcuticular tissues were closed with 2-0 Vicryl. Skin was closed using staples. Sterile dressing was then applied over the wound, and the patient was then transferred to the postoperative care unit in stable condition.
Post Operative:

Postoperative X-ray showing the AP view of the pelvis and the frog-legged lateral view of the right hip.
The postoperative recovery of the patient was unremarkable. She was prescribed aspirin 325mg for deep vein thrombosis prophylaxis.
She was allowed weight bearing as tolerated. Her pain was well managed with medications.
The patient underwent physical therapy to increase range of motion and flexibility. The home exercise program was started to increase the strength of the muscles.
After 3 months, the patient was walking without a cane and completely pain-free.
She was amazed at the outcome of the hip surgery. She had resumed her work as a florist and experienced no restriction in her activities.
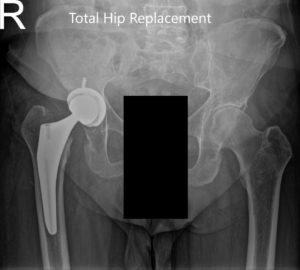
Postoperative X-ray showing the AP view of the pelvis and the frog-legged lateral view of the right hip (image-2)
The patient was happy returning to her baseline lifestyle. She now enjoyed riding her bicycle and playing with her grandkids without pain.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

