Case Study: Management of bilateral Hip Arthritis
in a 66-year-old Male with Total Hip Replacement
A 66-year-old male presented to our office for consultation regarding her bilateral hip pain for the past three years. The patient states about 2 years ago, his friend’s dog jumped on him from behind and made him fall forward, and when he tried to get the dog off, he felt a tear in his hip. The patient’s pain has been getting worse throughout the years.
The patient went to a previous orthopedic surgeon that told him he needs surgery but he didn’t want to perform surgery. The patient was previously working as a clerk at a bank and currently not working secondary to pain. He described difficulty in walking, standing for long, navigating stairs and activities involving bending, squatting and more recently even putting on his shoes.
The pain was described as dull in character which was greater on the right side. The pain was located in the bilateral groin radiating down to the inner knees with activity. The severity was moderate and constant in frequency. Recently, the pain was disturbing his sleep and he was emotionally disturbed from unremitting pain.
He had tried physical therapy, NSAIDs and hip cortisone injections with minimal relief. He was a past occasional smoker and a social drinker. He was currently on Flomax for benign prostate hypertrophy, Toprol XL for hypertension, and Lipitor for hypercholesterolemia. In the past, he had anterior cervical decompression surgery and right carpal tunnel release both done six years ago. He was allergic to penicillin.
The patient’s gait was antalgic, with a reduced stance phase on the right side. There was no evidence of scoliosis and exaggerated lumbar lordosis. Both the iliac spines, patella, and medial malleolus were at the same level. He was unable to squat or sit cross-legged.
On the supine examination, both the iliac spines were at the same level with no leg length discrepancy. The skin overlying bilateral groins was normal with no scar marks or sinus tracts. There was no fullness or swelling in the bilateral groin area. There were no enlarged inguinal lymph nodes.
Tenderness was present along the bilateral anterior hip joint line (right greater than left). The range of motion on the right was painful in rotation movements and restricted at end abduction. On the left hip, the range of motion was complete but with painful rotation movements. The straight leg raise test was positive bilaterally with pain in the bilateral groin. There was no coronal, rotational or sagittal plane deformity bilaterally.
Bilateral bulk and tone of muscles were normal. Light touch was intact in all sensory dermatomes of bilateral lower extremities. Examination of bilateral extremities revealed 5/5 power in all muscle groups. The bilateral lower extremity pulses were 2+ and comparable. The examination of bilateral ankles, knees was normal.
Imaging revealed osteoarthritic changes in bilateral hips (right greater than left). Considering the patient’s comorbidities and lifestyle limiting hip arthritis, he was advised bilateral total hip replacement. Risks, benefits, and alternatives were discussed with the patient at length. He decided to go for right hip replacement first.


Preoperative AP and lateral views of the right hip joint.

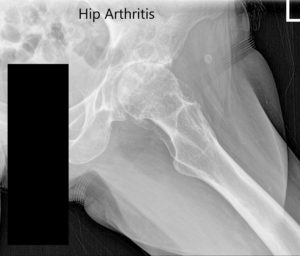
Preoperative X-ray of the left hip showing AP and lateral views.
OPERATION: Right total hip arthroplasty.
IMPLANTS USED: Ceramic femoral head 36 mm plus with127-degree neck angle system size 2, 30-mm neck length with a stem length 99 mm with a taper 54 mm cup with a 6 .5 mm screw 25 in length.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent, finding the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was then definitively positioned on the fracture table with the right hip up and the right hip was then prepped and draped in the usual sterile manner.
A curved incision centered over the greater trochanter was used for the arthrotomy. Skin and subcutaneous tissues were incised. The fascia was then divided. The hip was placed into internal rotation and the posterior soft tissue structures were then taken down and tagged for future repair.
The hip was then dislocated. The lesser trochanter to the center measurement was taken and the neck resection was made at the correct level. The head was then removed. Attention was then turned towards the acetabulum. The remainder of the labrum was then debrided. The acetabulum was sequentially reamed. The final shell was then placed into position in the correct abduction and anteversion.
A screw was used for additional fixation. Additional osteophytes were then removed. The poly was then placed over the shell. Attention was then turned towards the femur and the femur was then sequentially broached.
The final broach was left into position. The head was then placed over the trunnion. Hip was then relocated and trialed through a full physiological range of motion. The hip was stable in all physiological range of motion. Hip was dislocated. The combined anteversion was correct. The hip was then dislocated.
The trial components were removed. The final components were then placed into position. The hip was then relocated and the posterior soft tissue structures were then taken down and tied for future repair. A thorough lavage was given.
The injection was given. The fascia was then closed with Ethibond. Cutaneous tissues were closed with Vlcryl. Subcuticular tissues were closed with 2-0 Vicryl. The skin was closed using Monoderm. Sterile dressing was applied over the wound and the patient was then transferred to the postoperative care unit in stable condition.


Postoperative X-ray showing the AP and lateral views of the right hip.
Post-op he demonstrated no neurological deficit of the lower extremities. The pain was well managed with medications and aspirin was given for deep vein thrombosis prophylaxis. The patient was ambulatory with support and weight-bearing as tolerated. Sutures were inspected to be clean, dry, and intact.
Hip precautions were explained to the patient and rehabilitation was directed towards gait training and fall prevention. After three months of post-op, he was able to walk without support and reported zero pain on the right hip. The pain on the left side was reduced secondary to offloading.
The patient returned for a total hip replacement of the left side two months later. He was enthusiastic about the success of the right hip arthroplasty. He underwent a left total hip replacement with an acetabular shell of 52 mm and a 0-degree polyethylene insert. Additionally, a 6.5 mm x 25 mm cancellous screw was used for fixation. A ceramic head of 36 mm was used with a127 degree angle hip stem (stem length – 102 mm and neck length -30 mm).


Postoperative X-ray of the left hip showing AP and lateral views.
The patient’s recovery from left arthroplasty was similar to the earlier surgery on the right hip. After eight weeks of post-op, he reported zero pain in both hips, with intact distal neurological structures. The range of motion of both the hips was full. The patient was back to his baseline activity and mobility.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

