Case Study: Left Total Hip Replacement
in a 74-year-old Male
A 74-year-old Male Patient presented to our office with complaints of bilateral hip pain (left greater than right). He stated the pain started insidiously years ago located in the bilateral groins. The pain was especially worse on the left side and he used a cane for ambulation on his right side. He gave a history of traction and spica cast on the left hip as a child.
The pain was described as a dull pain that was radiating down to the left knee and left buttock. He described grinding sensation on moving his hip. The severity varied from moderate to severe with activity. The pain was constant and would get worse with activities such as walking, sitting, getting up from a chair, navigating stairs, bending, driving and prolonged standing.
He had previously tried conservative treatment such as physical therapy, heat pads, and received two hip joint injections with minimal relief. He was active before the pain increased and was anguished with his reduced mobility. He missed playing golf with his friends and going to the local restaurant.
He was a former smoker having quit 10 years ago. He denied any known drug allergies. His medical history was positive for hyperlipidemia, asthma, benign prostate hypertrophy, and high blood pressure. All his medical conditions were well controlled with medications. He had renal stone removal and right inguinal hernia repair done 10 years ago.
On physical examination, his gait was antalgic with a lurch and reduced stance phase on the left side. Left shoulder, anterior and posterior iliac spines were at a lower level than the right side., The bilateral patella and medial malleolus were at the same level. There was mild atrophy of the left buttock. The skin overlying the left hip was normal with no evidence of scar marks and sinus tracts. There was no bony mass palpable in the left gluteal region.
There was no exaggerated lumbar lordosis. There was mild functional scoliosis with convexity on the right side which disappeared on bending forward. There was tenderness in the left hip anterior joint line. Morris’s bi-trochanteric tenderness was negative. There was no thickening or broadening of the trochanter. There was no swelling/induration in the Scarpa’s triangle. The range of motion was restricted in abduction, extension, and internal rotation.
On squaring the pelvis there was no evidence of any fixed deformity. On digital palpation, the left greater trochanter was at a higher place than the right side. Apparent and true shortening were similar to 1.5 cm. The examination of the right hip, bilateral knee and ankles were normal. There was no distal neurological deficit and the bilateral deep and superficial tendon reflexes were intact. Bilateral lower extremity pulses were palpable and comparable.
Imaging studies revealed bilateral hip osteoarthritis which was severe in the left hip with dysplasia of the acetabulum. In view of lifestyle limiting hip pain, he was advised left total hip replacement. Risks, benefits, and alternatives were discussed with the patient at length. The patient agreed with the plan.
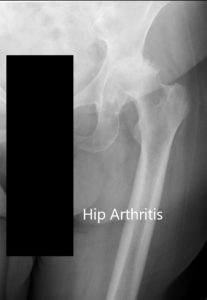
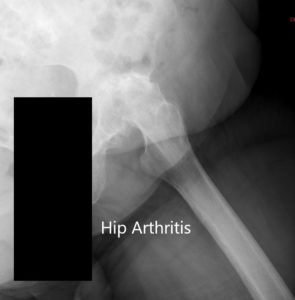
Preoperative X-ray of the left hip showing AP and lateral views.
OPERATION: Left total hip arthroplasty using ceramic femoral head 36-mm plus 5 with 127-degree neck stem system size 5 with a 54-mm acetabular shell cluster hole with polyethylene insert with two screws.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent, signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was brought to the operating room.
Anesthesia was obtained by the anesthesiologist. The patient was then definitively positioning with the left hip up and the left hip was then draped and prepped in the usual sterile manner. A curved incision centered over the greater trochanter was used for the arthrotomy. Skin and subcutaneous tissues were incised.
The fascia was then divided. Hip was then placed into internal rotation and the posterior soft tissue structures were then taken down and tacked for future repair. The hip was then dislocated. Lesser trochanter to center measurement was taken. The neck dissection was then performed.
Attention was then turned towards the acetabulum. The remainder of the labrum was then debrided. The acetabulum was then sequentially deemed. The final head was then placed into position and the correct abduction and anteversion. Screws were used for additional fixation. The poly was placed over the shell.
Attention was then turned towards the femur. The femur was sequentially broached. The final broach was left into position. Trunnion and head were placed and the lesser trochanter to the center measurement was taken and was found to be correct. Hip was relocated and trialed to a full range of physiological motion and hip was stable in all physiological range of motion.
The combined version was found to be correct. Hip was then dislocated. The trial components were then removed. The final components were then placed into position. Hip was then relocated. Thorough lavage was given. Posterior soft tissue structures were then tacked to the greater trochanter through transosseous tunnels.
The fascia was closed with Ethibond. Cutaneous tissues were closed with Vicryl. Subcuticular tissues were closed with 2-0 Vicryl. The skin was closed using staples. Sterile dressing was then placed over the wound, and the patient was then transferred to the postoperative care unit in stable condition.
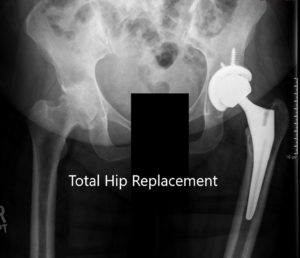

Postoperative X-ray showing the AP view of the pelvis and lateral view of the left hip.
The recovery was excellent with pain managed with medications. The abduction pillow was advised and hip precautions were explained to the patient in detail. Weight-bearing was allowed with support. Aspirin was prescribed for deep vein thrombosis prevention.
The sutures were removed on 14th-day post-op. The wound was healthy, clean, dry and intact. The patient was advised to continue physical therapy, gait training, and fall prevention education. On three months follow up, he demonstrated a pain free gait, full range of motion. Aspirin was discontinued and he was advised to slowly wean off hip precautions.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

