Case Study: Medial meniscus repair and
Patellofemoral chondroplasty in a 33 year-old male
The main purpose of medial meniscus is to lessen the strain on the knee joint. The ragged edge of an unchecked meniscus tear may become stuck in the joint and cause discomfort and edema. Also, it may result in permanent knee issues including arthritis as well as other ligamentous harm.
Since the damaged cartilage can cause the knee to become unsteady, create discomfort and inflammation, or cause the knee to lock-up or become stuck, many persons with torn meniscus choose to have surgery.
The damaged meniscus in your knees can be removed through an outpatient procedure called a meniscectomy. Often, an arthroscopic operation is used to complete it. This procedure includes making a centimeter-long incision to insert a minimal invasive camera called an arthroscope and other small devices to remove all or part of the meniscus.
A surgery called chondroplasty is used to replace and remodel worn-out cartilage in joints. Degenerative cartilage is smoothed throughout the treatment, and any unstable cartilage flaps are trimmed.
A 33-year-old patient was in our office with complaints of the left knee. He had 2 episodes of buckling 6 weeks back. He is in constant severe pain, and he has been limping. He heard a crunch at the time of buckling but no history of locking.
Pain is worsened with stains, deep knee bends, and a change of position which is associated with swelling. He has no past medical history and no known allergies. He does not take anything for the pain.
Upon examination of the left knee, the patient is tender to palpation along the medial joint line and has an effusion. They are tender to palpation along the medial and lateral facets of the patella. They have crepitus of the patellofemoral joint with range of motion and discomfort with patella grind testing.
The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They have limited range of motion. They have 5/5 strength and are neurovascularly intact distally. There are no erythema, warmth or skin lesions present.
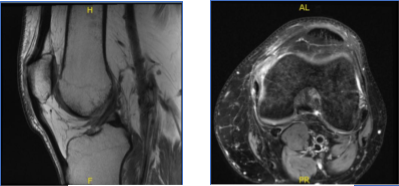
MRI-3T Left Knee Non-contrast
Results for MRI were presented and shown sprain of the medial collateral ligament, without evidence of high-grade tears. Longitudinal vertical tear involving the outer third of the body and posterior horn medial meniscus.
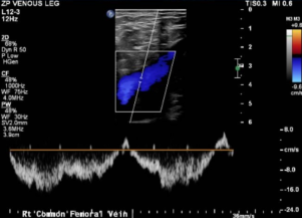
Doppler Venous Left Lower Extremity
Normal Doppler venous examination of the left lower extremity. There is no evidence of deep venous thrombosis.
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections, and surgical options.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
We talked about the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal.
We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol. We discussed arthroscopic Left knee partial medial meniscectomy and chondroplasty.
The patient was taken to the operating room where he was placed on a well- padded operating table. General anesthesia was induced. A mid-thigh tourniquet was applied on the left lower extremity. The left lower extremity was exsanguinated using an Esmarch and the tourniquet was elevated to 350 mmHg.
The left lower extremity was prepped and draped aseptically using chlorhexidine paint. A lateral working portal was established over the left knee. The scope was entered, and examination of the knee was performed. There was patellofemoral arthritis on the medial side of the patella. There was grade 1 to 2 patellofemoral arthritis on the medial facet of the patella.
There was grade 1 to 2 arthritis of the medial femoral condyle. A bucket-handle medial meniscus tear involving the posterior horn was seen going up to, but not involving, the posterior root. The scope was entered into the intercondylar area and the tear could be evaluated.
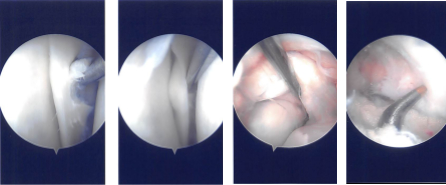
Intraoperative Arthroscopy Images
The intercondylar area was examined and the acromioclavicular ligament was found to be intact. The lateral femoral condyle was examined, and the lateral meniscus was intact. There was no cartilage damage on the lateral femoral condyle.
Now the repair of the bucket-handle tear of the posterior horn of the medial meniscus was started using FasT-Fix. Four FasT-Fix were used and taking bite, the peripheral and then the central part of the meniscus was performed.
The suture was cinched and tightened to find the good reduction of the tear. The tear was opposed well after the use of the four FasT-Fix. The chondroplasty of the patella was also done. The knee was irrigated and washed.
The closure was performed using #4-0 nylon. Dressing was done using Adaptic, 4 x 4, Webril and Ace wrap. The tourniquet was removed. Knee immobilizer was applied on the left knee. The patient was extubated and moved to the postoperative holding area in a stable condition.
The patient is to ambulate with crutches, with partial weight bearing on the left lower extremity. He is to always use a knee brace when ambulating. He can loosen the brace while sleeping. He can remove the brace while he is resting. He is to follow up after a week for suture removal, re- evaluation, and start of physical therapy.
The patient visited after a week for his postoperative follow up with complaints on his left knee meniscus repair and chondroplasty. Patient had increased pain. He buckled after his dog ran on him.
Results for his MRI were presented and show no findings to suggest new internal derangement of the left knee. Resolution of previously seen edema associated with the previous medial collateral ligament sprain. Unchanged appearance of a peripheral vertical tear through the posterior horn of the Medial meniscus with minimal generalized medial compartment chondromalacia.
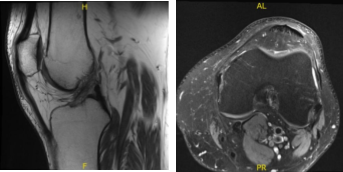
MRI-3T Left Knee Non-contrast
After a few months the patient visited for a follow up and presented the results of his MRI and shown signal alteration the posterior horn medial meniscus may represent a site of primary repair of the medial meniscus tear. Correlate with surgical history. No new tear is visualized. Trace joint effusion. Small quadriceps enthesophyte.
MRI-3T Left Knee Non-contrast
The patient undergoes a surgery again after a month for meniscal repair and meniscectomy. The patient was taken to the operating room and placed on a well-padded operating table. Three grams of Ancef was given. General anesthesia was induced.
The left lower extremity was prepped and draped aseptically with the tourniquet. The tourniquet was elevated after application of Esmarch. Lateral working portal was made in a usual fashion. The scope was entered and a patellofemoral joint was examined. There was a condylar lesion on the medial inferior patellar facet.
The medial gutters were cleaned. Medial tibiofemoral compartment was entered where there were grade 1 to grade 2 lesions. Posterior horn of the medial meniscus showed tear and fraying. A medial working portal was made.
The tear was reexamined and found to be a peripheral tear through the suture with free margins. Shaver was Introduced and frayed margins excised as weak as meniscus and capsule roughened to prepare for repair.
Intraoperative Arthroscopy Images
The scope was moved to the intercondylar area where ACL was found to be intact. Partial synovectomy was performed in that region. The scope was moved to the lateral femorotibial compartment where the left meniscus was intact. no chondral damage to the lateral femoral condyle.
Then, the scope was reentered into the patellofemoral joint where the trochlea was found to have grade 1 condylar lesions. No chondroplasty was performed on the trochlea. There were grade 2 to grade 4 lesions on the inferomedial patella facet. Chondroplasty was performed.
Now, the scope was moved from the lateral to the medial working portal. The lateral working portal was clean and using a shaver to make easy access to the medial meniscus.
Zone specific cannulas were reused to pass sutures through the medial posterior horn and body of the medial meniscus through the capsule. Three horizontal and one vertical mattress suture were used. They were held firmly and found to have made a good reduction of the meniscus
Now, the scope was removed, and a posteromedial incision was made just posterior to the MCL. Saphenous nerve was seen and retracted free. A blunt dissection was done behind the capsule and the sutures were retrieved. The sutures were tightened consecutively from posterior to anterior.
Tightened and knotted. Once it was done, the scope was reentered and found to have a satisfactory repair. (07:58) were used to make four holes in the intercondylar notch anterior to the ACL attachments.
Fat globules could be seen. The tourniquet was released and blood could be seen coming out of those holes. The scope was removed, and the knee was thoroughly washed and irrigated.
Hemostasis was achieved on the posteromedial incision. Closure of the wounds were done in layers using #2-0 Vicryl and #3-0 Monocryl. Dressing was done with Steri-Strips, Adaptic, 4×4, Webril, Ace wrap. A knee immobilizer was applied. The patient was extubated and moved to recovery in a stable condition. Post Op examination showed no neurovascular deficit.
After discussing the options for treatment and the risks of aspiration and injection, the patient wished to proceed with the aspiration and injection to reduce pain and swelling.
After a sterile prep, and the injection of a local anesthetic, 90 cc of straw-colored fluid was aspirated from the left knee joint. This was followed by an interarticular injection, consisting of 60 mg or Toradol followed by 1cc of 1% lidocaine, 1cc of 0.5% Marcaine.
The patient tolerated the procedure well and there were no complications. Post aspiration pain, and the signs of infection were discussed in detail. Patient checked in for follow up visit after a month and seen significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.