Case Study: Knee Arthroscopic: Lateral Meniscectomy and
Chondroplasty of the Patella and Medial Femoral Condyle
in a 34-year-old female
In order to treat kneecap fractures, which are a frequent but devastating injury, patients are often immobilized or, in rare circumstances, undergo surgery. The bones of the knee can dislocate. An impact at high speed, a tumble, or an accident might cause this to happen.
One of the possible ways yet uncertain is to undergo a surgery. During a knee arthroscopy, a surgeon uses a tiny instrument called an arthroscope to examine and treat issues. It is a less intrusive kind of surgery used to identify and address joint problems.
A 34-year-old patient was in our office, with complaints of left knee pain. The patient had gone to the ER to place knee back into the socket, she stated leaving the ER, there was no more pain. She said used to pop her knee back into place, by herself.
Patient describes the pain as sharp, dull, stabbing, throbbing. The pain is associated with swelling, bruising, numbness, tingling, and radiating pain but not associated with weakness, bowel or bladder abnormality, gait problem, giving way, or limping, hand function difficulty.
However, bending makes the symptoms worse. Using a knee mobilizer makes the symptoms better. The patient has undergone surgery for the left knee, carpal tunnel, and c-section. Patient does not smoke. She works for cleaning services and is not able to work without considerable pain at present.
Upon examination of the left knee, the patient is nontender to palpation along the medial and lateral joint lines and has mild effusion. They are tender to palpation along the medial aspect of the patella and medial patellofemoral ligament.
They have no crepitus of the patellofemoral joint with range of motion but are apprehensive to patella glide testing. The patient has no discomfort with McMurray’ s maneuvers, and the knee is stable. They have limited range of motion.
They have 5/5 strength and are neurovascularly intact distally. There are no erythema, warmth or skin lesions present. On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability, and strength.
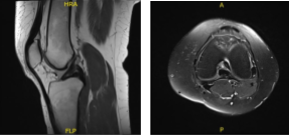
MRI results were presented and shown single slice visualization of a small medial meniscus tear. Trace joint effusion. The ACL is unremarkable, without evidence of tear, degeneration, or postoperative change.
MRI -3 T Left Knee Non-contrast
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
The patient has expressed a desire to proceed with surgery. I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome.
Understanding there is a long rehabilitative process that typically follows the surgical procedure, and the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return.
The patient also understands the risks of re-tear or failure to heal. The patient expressed understanding of these risks and has elected to proceed with surgery. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol.
The patient was taken to the operating room area where she was put on a well-padded operating table. General anesthesia was induced.
Left lower extremity was prepped and draped aseptically. Preoperative antibiotic was given. Lateral entry portal was made for the arthroscopic examination. The arthroscope was inserted.
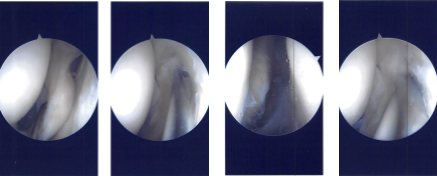
There was a small patch of grade 2 to grade 3 arthritis on the medial patellar area, which was cleaned. Examination of intercondylar notch was intact ACL. Examination of the tibiofemoral joint medial marginal meniscus, which was cleaned using shaver and upbiters. There was no tear in the medial meniscus.
There was a large popliteal hiatus with the possible tear going into the posterior horn of the lateral meniscus, which was incomplete. A thorough examination was done, and the debridement was done. The decision was made not to repair it at present because it seemed to be an extensional popliteal hiatus.
Intraoperative Arthroscopy Images
Now the scope was removed, and medial incision was given over the superior medial margin of the patella. Tendon was exposed and cleaned Two guidewires were passed under C-arm.
Reaming was done over the guidewire and placed for the SwiveLock. Another guidewire was passed in the patella about 15 mm distal. Remaining was also performed.
The free end of the tendon was inserted into the patella on the superior and inferior holes using SwiveLock. Now the femoral point was found using a guide and Incision was given after checking under C-arm. The dissection was reached.
A guidewire was placed again and checked under C-arm and found to be in the appropriate position. It was put into the femoral and from medial inferior to posterior superior direction.
The dissection was done between the second and third layer of the medial knee at the patella and tonsil was reduced and passed onto the femoral site.
The suture was passed back from there and the tendon was passed back into the femoral site and delivered. It was tied around the wire and found to be in an acceptable position which was tied in 30-degree flexion and loosened in 90 degrees of flexion as well as extension. Reaming was performed. The Beath pin was passed through and through.
Reaming was performed from 40 mm over the Beath pin. The sutures through the tendon loop were passed through the Beath pin and passed out laterally. An appropriate tension not to over tighten the patella was put with 30 degrees of flexion and excision of the tendon was done with Interference screw. Final tendon was checked and found to be satisfactory.
The sutures were removed, and the patella sutures were used for reinforcement and cut. Closure of the wound was done after irrigation in layers. Monocryl was used for closure. Dressing was done using 4 x 4, ABD, Webril, and Ace wrap. Bledsoe brace was applied and was put in extension.
The patient was extubated. Femoral canal block was done by the anesthesia for pain relief. The patient was informed preop about that as well as optimal injury to her mother about the precautions as well as the use of brace. The patients asked to use the medication, ice, and elevation.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for follow up visits after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.